Image credit: Laura M. Lombardía / CNIO
News • Research on physical conditions
Exploring the link between obesity and cancer risk
Being obese or overweight increases the risk of developing several types of cancer, but the reason why is not clear.
Obesity or overweight might not even be a direct cause of that increased risk. Some research suggests that its origin lies in the alterations they cause, or perhaps in changes in the body induced by these physical conditions. Understanding the relationship between obesity, overweight and cancer is key. The National Cancer Research Centre (CNIO) is exploring this issue through the groups led by Guadalupe Sabio, Nuria Malats and Héctor Peinado.
According to the 2020 European Health Survey, in Spain 16.5% of men and 15.5% of women over 18 years of age suffer from obesity, and overweight affects 44.9% of men and 30.6% of women. Guadalupe Sabio leads CNIO’s Organ Interaction in Metabolic Diseases Group, which studies the relationship between cancer and obesity: “Epidemiological studies showing a very strong relationship mainly with liver and colon cancer – also with others, but with smaller statistical evidence – first began in 2010. Shortly after, the phenomenon was studied in animal models and it soon became apparent that those with a high-fat diet show a propensity for liver cancer, a relationship that was also seen later with other tumours types.”
Recommended article

Article • Awareness
Focus on cancer
From solid tumors to metastatic carcinomas and leukemia: cancer is among the most common causes of death. Keep reading for latest developments in early detection, staging, therapy and research.
One of the tissues that is most damaged with obesity is adipose tissue – fat, present in the typical ‘spare tyres’. Sabio’s group discovered a certain type of protein that is very active in obese people. If removed from adipose tissue, the risk of cancer is reduced. “We found that when we removed them from the adipose tissue of animals, they had a lower risk of developing liver cancer. From there we started studying what those proteins are like in people.” Sabio began analysing these kinase proteins, differentiating between “obese and thin people and, something that had not been done before, between women and men.” What they discovered was that this route is less active in women than men. “This was a very significant fact, because men are four times more likely than women to develop a liver tumour,” explains Sabio.
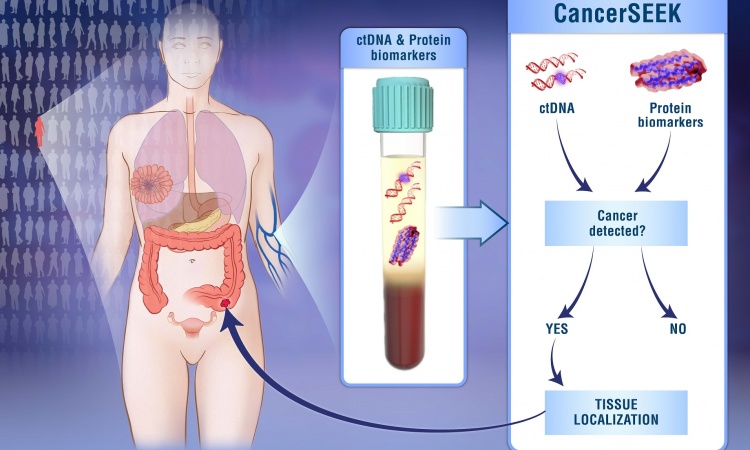
This group is now investigating how fat affects other types of cancer, such as breast cancer, and continues to look for fat-related blood biomarkers that tell us if a person is at higher risk of developing liver cancer.

Image source: Amparo Garrido / CNIO
Núria Malats, who heads up CNIO’s Epidemiology and Molecular Genetics Group, has led a large international study, PanGenEU, dedicated to investigating the factors associated with pancreatic cancer risk. The ultimate objective is to establish screening programmes that allow for early detection of the disease. Pancreatic cancer is often detected in its advanced stages and usually causes death within a year of diagnosis, so it is crucial to improve early detection. “Pancreatic cancer is strongly associated with obesity as a risk factor,” Malats explains. But the relationship is not yet understood: “We believe the role of obesity is much more complex and we think there are other related factors.”
The group led by Malats had already shown that long-term type 2 diabetes is a risk factor in pancreatic cancer. “We believe that diabetes mediates the effect of obesity, and obesity mediates the effect of diabetes, and neither factor is causally linked to pancreatic cancer. This suggests that preconditions leading to both diabetes and obesity may be the cause of this increased risk of pancreatic cancer.” These preconditions could lead to mild and chronic inflammation of the pancreas, which would induce diabetes and obesity and eventually pancreatic cancer. “The causes of this inflammation might be genetic or related to the microbiome, the community of microorganisms that inhabit our bodies,” says Malats. It is a line of research she is exploring with CNIO’s Epithelial Carcinogenesis Group , led by Paco X. Real.
On the one hand, obesity increases what is known as vascular permeability. And we have seen that in organs where there is metastasis, vascular permeability also increases
Héctor Peinado
Héctor Peinado, head of CNIO’s Microenvironment and Metastasis Group, is investigating the relationship between obesity or overweight and metastasis, the process by which a primary tumour reproduces in other organs and spreads through the body. Little is currently known about this: “It seems clear that obesity influences the spread of cancer, but research has not focused, until now, on explaining at the molecular level why this happens,” Peinado explains. This is what he began to investigate in 2015. “We started with melanoma, and we saw that in obese mice cancer cells metastasise better. Then we moved on to breast cancer, where the risk is more closely related to obesity than melanoma. Also in this case we found that cancer cells metastasised better in obese mice. So we already had evidence for two types of cancer: melanoma and breast.”
With these data, the group established a hypothesis: “We believe that obesity affects the organs in which cancer metastasises. On the one hand, obesity increases what is known as vascular permeability. And we have seen that in organs where there is metastasis, vascular permeability also increases,” says the researcher. “Another change that obesity causes is the increase in platelet activity, and we see that in our mouse models, in their organs with metastases. It seems that the tumour cell takes advantage of these two circumstances to nest and form metastases.”
Peinado is now turning his attention to humans: “We are collaborating with Miguel Quintela’s group, from CNIO’s Breast Cancer Clinical Research Unit, to try to extrapolate our observations to patients. Our hypothesis is that obesity systemically influences metastasis, and we are looking for ways to control or reverse it.”
In mouse models, diet change strategies have proven to be effective: “We are testing therapeutic strategies on our mouse models. For example, switching from a high-fat diet to a normal diet. This, extrapolated to a patient, would mean eating a healthier balanced diet instead of saturated fats and processed foods. The data suggest that a change in diet could reduce tumour cells’ metastatic capacity. And we are also using platelet aggregation inhibitors that reduce this metastatic nesting capacity,” explains Peinado.
Furthering our knowledge of the relationship between obesity/overweight and cancer is fundamental in oncology. According to the National Cancer Institute in the United States, between 2011 and 2015 there were 37,670 new cases of cancer in men and 74,690 in women that were related to excess body weight (in Spain there are no specific data). In addition, between 2005 and 2014 most cancers associated with overweight and obesity increased by 7% in the US, while cancers associated with other factors decreased by 13%.
The National Cancer Institute (NCI) recognises that there are thirteen types of cancer whose risk increases with obesity or overweight in varying proportions:
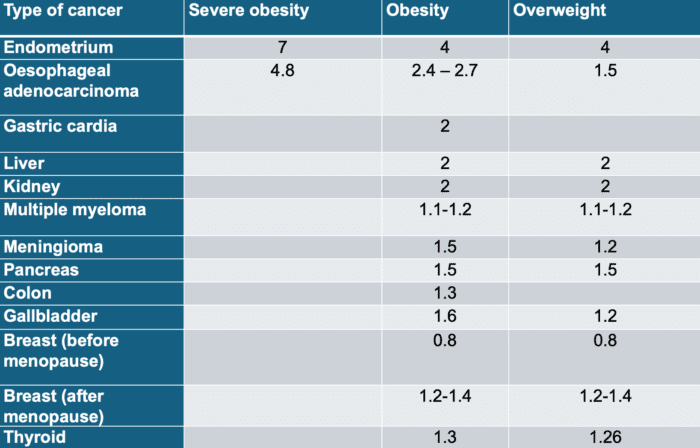
Image source: CNIO
In addition, each 5-unit increase in the Body Mass Index (BMI), which is the indicator of obesity and overweight, increases the risk of breast cancer after menopause 1.2-fold and ovarian cancer 1.1-fold.
Source: Spanish National Cancer Research Centre
05.07.2024