Colorectal cancer today and tomorrow
Colorectal cancer (CRC) jointly describes cancers of the colon and rectum. Worldwide, CRCs are among the most common cancers. In Europe and the USA the occurrence of CRCs are considerably higher than in Africa and Asia.

In Europe, the highest occurrence rate is in Germany, which registers over 70,000 new cases annually. The difference in the occurrence of the disease in men and women is scant – with 17.4% female and 16.3% male, the disease is ranked second after breast cancer and prostate cancer respectively.
Meike Lerner asked gastroenterologist, haematologist and internal oncologist Professor Stephan Petrasch, head of the Internal Medicine department at Wedau Clinic in Duisburg, for possible reasons behind this country’s negative CRC record; gender-specific differences in diagnosis and therapy, and the advantages of current treatments as well as potential advances
Prof Petrasch: ‘We have the most aggressive strategy for prevention: Every man and woman aged 55+ is entitled to a colonoscopy every 10 years, which is fully covered by the medical insurers. Additionally, the awareness of the disease in Germany is high. Therefore the acceptance of prevention is high and, consequently, so are the number of carcinoma cases detected at an early stage. So, although this means that over the last few years more incidences of colon cancer were detected, the mortality rate from CRC has actually simultaneously decreased because the disease is often detected at a treatable stage. This is the difference between Germany and other countries, where this kind of prevention is not offered and patients are only examined after symptoms have begun to occur – at which stage the cancer will have progressed much further. The sigmoid colonoscopy, carried out in the USA, for example, misses out the upper parts of the large intestine and is carried out by nurses – which may also be a reason for the lower incidence of CRC detected there.’
Are the attitudes of men and women different towards prevention?
‘Yes. It’s estimated that twice as many women than men take advantage of preventive colonoscopy. There are several reasons for this: because of mammography screening programmes and smear tests, there is more sensitisation among women for preventive examinations. In addition, gynaecologists actually support us because they tend to remind women about preventive colonoscopy during their examinations. Men are not subject to this “control mechanism”; in addition, they generally tend to view a visit to the doctor as a sign and admittance of weakness and are less often prepared to see a doctor.’
What preventive examinations are available and how should they be rated?
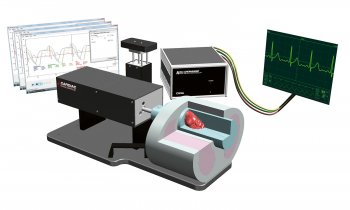
‘Colonoscopy is still the state-of-the-art, preferred method of examination because it’s the most precise procedure and because polyps can actually be removed while the examination is carried out. The disadvantage of colonoscopy is that the examiner cannot see the areas behind the intestinal folds. Virtual colonoscopy, via MRI or CT-colonography, is less invasive. Additionally, it delivers reproducible images with the advantage that the regions behind the intestinal folds are clearly visible. However, polyps with a diameter of less than 1cm cannot be detected, and neither can flat adenomas, which have the highest potential of malignancy. These are best detected through a combination of colonoscopy and magnifying or chromoscopic colonoscopy. Moreover, neither CT nor MRI is suitable for comprehensive screening, as offered in Germany: CT must be ruled out because of the radiation exposure, MRI because of the high complexity and costs. Another reason is that for a good MRI or CT the bowels would have to be completely empty because any remaining stools can imitate polyps.
‘Capsule endoscopy is a new procedure. The patient swallows a capsule with two miniature cameras that move through the bowel in a natural way. The capsule transmits data to a receiver attached to a belt the patient wears. Data from this receiver is then transferred to the PC. However, the capsule cannot be navigated and ‘overlooks’ changes in the large intestine more frequently than other procedures. Therefore we only use the capsule for patients who have had bad experiences with colonoscopy, or who cannot undergo a colonoscopy because they take blood-thinning medication. However, over the next few years I think it is likely that a lot of progress will be made with capsule endoscopy for colon diagnosis, because this procedure holds a lot of promise for the future.
What about the Haemoccult test (FOBT)?
‘This is offered as a matter of prevention in many other European countries, but it has neither the necessary specificity nor sensitivity obtained, for instance, through the PSA test for prostate cancer. This is another reason why in many European countries CRC is only detected at an advanced stage.’
Are there any new procedures for the early detection of colon cancer?
‘Currently, colonoscopy is extended through “third-eye” technology – we insert an additional optical instrument through the endoscope, which is rotated by 180 degrees and makes the rearward areas of the intestinal folds visible. This would solve the current shortcoming of colonoscopy. However, this is still in the trial stage, but the technology is likely to become established soon.’
Are there gender-specific differences from diagnosis to therapy?
‘No, treatment is the same for men and women.’
What progress has been made in CRC treatment?
‘The changes over the last 10 years have been spectacular. Whereas ten years ago we only had 5-Flourouracil available, in 2000 new chemotherapeutics, such as Oxaliplatin and Irinotecan, came on the market, which improved survival rates and response rates considerably. From 2005 biologicals have been available for treatment: antibodies that stem the growth of vessels, and antibodies that impact on the growth receptors on the cell surface. Moreover, surgery for metastases following neo-adjuvant chemotherapy, or for directly operable metastases, has become a decisive factor. Today the chance of a cure for patients with metastasising CRC after successful surgery is 25%.
‘Through new chemotherapeutics and antibodies the five-year survival rate for patients with metastasising CRC has increased from 14 months to more than 20 months. We expect another 40-50 drugs to be licensed over the next few years, which will further change these levels.’
16.09.2009