Article • Boosting our immune surveillance
Antibodies PD-1 and PD-L1: a quantum leap in cancer therapy
Immuno-oncology is a therapy in which the body’s immune system treats a tumour. Dr Eric Borges, from the Research and Development Centre at Boehringer Ingelheim Pharma GmbH in Germany, explains why this is revolutionary.

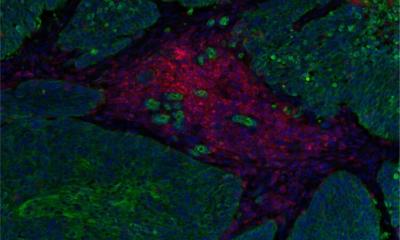
© Boehringer Ingelheim
"Unlike conventional cancer therapies, with immuno-oncology the tumour cell is not the direct target, it’s the patient’s immune system. The medication stimulates this to then fight the cancer cells. The immune system is trained to detect foreign structures in the body and to remove them. Bacteria, viruses, toxins – it detects anything foreign and destroys it. With immuno-oncology we try to impact on the immune system so that it recognises tumour cells as being foreign and destroys them.
With conventional cancer treatments we have used our cancer cells findings to develop new drugs. As cancer cells divide faster than most normal cells, we developed chemotherapeutic agents that destroy the fast-growing cells. The discovery of tumour-relevant mutations in cancer cells was utilised to develop targeted drugs to neutralise the effect of such mutations. Unfortunately, tumour cells frequently find ways to elude the effects of these drugs and develop resistances. The immune system, however, reacts immediately to changes in the cancer cell. It can adapt to the changed situation and so can better prevent the development of resistances.
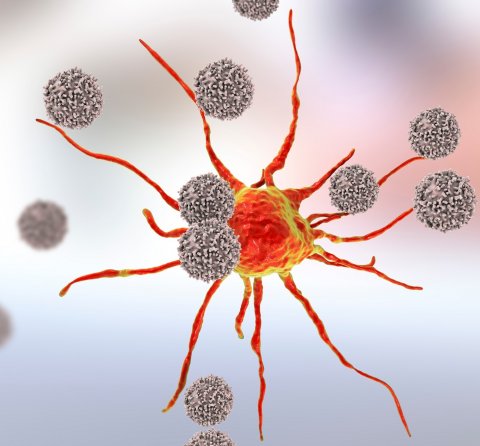
Melanoma cells usually have many mutations and are therefore easy to detect by the immune system. But, the cancer still manages to elude this immune surveillance. The tumour generates an environment that strongly reduces the activity of the immune cells, so they can no longer attack them – so the melanoma grows. So-called ‘checkpoint inhibitors’ have been available for a while, primarily monoclonal antibodies against PD-1 and its ligand PD-L1, which neutralise one of the essential immune-suppressing mechanisms of the tumour. This causes the tumour-specific immune cells to become active again and to attack and destroy the tumour cells. These PD-1 and PD-L1 specific antibodies represent a quantum leap in cancer treatment, and their potential, combined with other therapeutic agents, is being trialled in more than 1,000 clinical studies. These antibodies are currently licensed to treat many cancers, including melanoma, lung, kidney and bladder cancers, and also certain types of lymphoma, bowel or uterine cancer.
Presently, we see the most success with ‘hot’ tumours. But there are also high expectations for the development of improved chances of cures for cold tumours. In immuno-oncology we distinguish between ‘cold’ and ‘hot’ tumours. We refer to tumours as hot when the appropriate immune cells are already located in the tumour and only the local immune-suppressing effect of the tumour cells prevents the immune reaction. When this blockade is lifted, through PD-1 or PD-L1 antibodies for instance, the immune system can take control and remove tumour cells.
Immunotherapy – a breakthrough
Patients who respond to this treatment have real chances of becoming free of symptoms, or possibly even tumours, for many years. Some tumours have been gone for more than ten years, even those with such life-threatening diseases as black melanoma. This has only been observed in a small number of patients treated, but immunotherapy could increase the chances of real cures for cancer significantly. At the moment it applies mainly to patients whose tumours have high mutation rates, which can be classed as ‘immuno-active’ or ‘hot’ types of tumours that benefit from immunotherapy – including melanoma. Its development is strongly favoured by increased UV exposure, i.e. sunbathing without sunscreen, which can lead to a concentration of skin mutations, and later to degeneracy of the mutated cells, i.e. a cancerous growth.
Recommended article

Article • Immuno-oncological biomarkers
Seeking to augment the value of tumour infiltrating lymphocytes
Measuring tumour infiltrating lymphocytes (TILs) is gaining importance in immunotherapy, but other variables must also be considered to boost prognosis and prediction accuracy, a leading pathologist argued at EBCC 11 last March in Barcelona. When it comes to prognosis and prediction for immunotherapy, a potentially new variable is emerging – TILs – white blood cells that have left the blood…
From cold to hot
The biggest success with cold tumours is likely to be achieved with combination strategies
Eric Borges
However, where these PD-1 antibodies and therefore immunotherapy in its current form does not work is in cold tumours. They contain none, or only few, immune cells and therefore the tumour has no inflammatory reaction. The challenge will be to heat up these cold tumours so that currently available immunotherapies will also work. There are many concepts for this in preclinical or early clinical studies; with most this amounts to combination therapy, with one drug primarily changing the cold tumour into a hot one and the second drug neutralising the local immunosuppression.
We are literally going through a very hot phase; researchers are experimenting a lot. Among others, we are testing small molecules, antibodies, cytokines, oncolytic viruses and vaccines, i.e. everything that’s suitable for the generation of an efficient immune reaction against the tumour cells. Research is intense in this field – I hope we’ll see many more breakthroughs in the near future.
Immunotherapy limitations
These are seen in treatment of cold tumours. One of the coldest types of cancer is pancreatic cancer; many cases are still fatal. Breast cancer and prostate cancer are also colder tumours – but, basically, cold tumours can be seen in almost all indications. Immunotherapy is therefore not so much aimed at the different indications but at the immune and mutation status of individual tumours. In other words: Each tumour indication will only ever have a certain rate of response for immunotherapy. For instance, melanoma is currently around 40%. This means, unfortunately, that the other 60% will not respond. For lung cancer the rate of those responding to existing immunotherapy with PD-1 antibodies is currently only around 15-20%. Combined with chemotherapy though the response rate is considerably higher. Therefore, we are hopeful that further combination therapies will continue to increase the success of immuno-oncology and will facilitate better treatment options for patients.
The differentiation between hot and cold applies to all cancer types. For skin cancer, the proportion of hot tumours is around 40%, for bowel cancer around 10-15%. For pancreatic cancer it’s extremely low. We are working to increase this rate with new treatments and I’m convinced a lot will happen in the next five years. The biggest success with cold tumours is likely to be achieved with combination strategies.
Recommended article

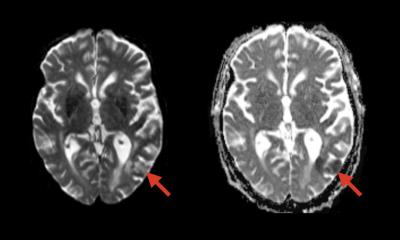
Article • Cancer pseudoprogression
Immunotherapy: Bigger lesions, better outcomes
With immunotherapy, bigger lesions may be spotted on CT, but it doesn’t necessarily mean that the disease is progressing. As treatment works, it can cause what has become known as pseudo disease progression; and this is just one of the many revolutions immunotherapy is triggering in oncology imaging, Professor Clarisse Dromain (Lausanne/CH) explained as she opened the session dedicated to this…
As with HIV, might cancer become a chronic disease?
I’m convinced this objective is realistic – with one difference. With current HIV treatment, patients must take medication for a lifetime to prevent disease recurrence. However, after successful treatment, immunotherapy can be stopped without the tumour starting to grow again. In some cases, patients have remained tumour-free for more than ten years after treatment ends. This is because functioning immune surveillance prevents renewed tumour growth. However, patients free of symp-toms for many years after successful immunotherapies is still small in number – melanoma is around 10%; lung cancer significantly lower.
This is the second big difference to anti-viral treatment as used in HIV therapy: With cancerous diseases we are looking at very heterogeneous disease patterns, where individual patients respond in very different ways to the same type of treatment. Our objective will be to develop a wide range of highly effective immunotherapeutic agents while simultaneously gaining a better understanding of which drugs promise the best treatment options for the respective patients."
Source: www.pharma-fakten.de
24.06.2019