© Sebastian Kaulitzki – stock.adobe.com
News • Success of aRCC treatment
New biomarker to better predict immunotherapy response in kidney cancer
Every year, nearly 2,000 people in Belgium are diagnosed with kidney cancer. Thanks to immunotherapy, survival rates for metastatic kidney cancer have increased dramatically in recent years:
More than half are still alive five years after diagnosis, compared to only 10% in the past. Unfortunately, the innovative treatment does not work for all patients. To investigate why there is such variation in the efficacy of immunotherapy, and in the hope of better predicting in which patients the treatment will succeed, a Leuven research team set up a large retrospective study. They analysed many samples from kidney cancer patients treated with immunotherapy at UZ Leuven over the past decade.
The researchers published their findings in the journal Nature Medicine.
The new insight that the interaction between certain T cells and macrophages is important for the success of immunotherapy opens up interesting avenues for future treatments
Benoit Beuselinck
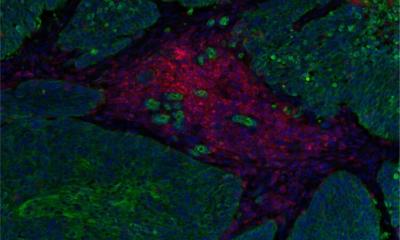
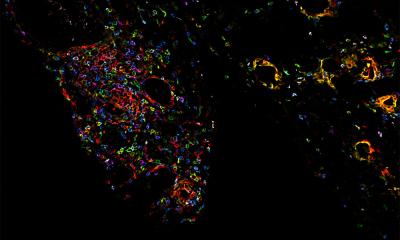
Doctoral researcher and oncologist in training Dr Lisa Kinget and postdoc Stefan Naulaerts: "We examined both tumour biopsies and blood samples with advanced laboratory techniques. Via machine learning, we combined gene expression in the tumour with hereditary characteristics of the patients' immune system, more specifically the HLA genes, which come in hundreds of variations depending on the individual. This approach allowed us to find a 'molecular signature' that showed a clear association with clinical response and survival rates. We further confirmed this association on independent samples from more than 1,000 kidney cancer patients from other international studies."
The lab analyses further showed that a successful response to immunotherapy was tied to a good interaction between two types of immune cells, namely CD8+ T cells and macrophages. Prof Abhishek D. Garg, KU Leuven: "Previously, researchers mainly looked at immune cells at the level of individual cell types, which led to oversimplified biomarkers. As a result, we thought macrophages were 'bad' for immunotherapy. With this study, we show that the interaction between different types of immune cells in a specific spatial context is more important in fighting kidney cancer."
Prof Dr Benoit Beuselinck, medical oncologist at UZ Leuven: "In the future, we hope to be able to use our method as a biomarker to predict in which patients immunotherapy will be effective. The new insight that the interaction between certain T cells and macrophages is important for the success of immunotherapy opens up interesting avenues for future treatments. We are currently busy setting up new clinical trials of combination therapies to stimulate both cell types and make them work better together, which may be more effective than current treatments."
Source: UZ Leuven
28.05.2024