News • Cancer care
Remote 24-hour monitoring shows promise in chemotherapy patients
Remote 24-hour monitoring for cancer patients receiving chemotherapy helps to better manage side effects and improve quality of life, finds a study published by The BMJ.
The researchers say remote monitoring can provide a safe, secure, and “real time” system that optimises symptom management and supports patients to remain at home - and is particularly relevant in the context of the Covid-19 pandemic. Effective symptom monitoring and management is essential during chemotherapy for cancer, but current approaches rely on patients recognising that symptoms are severe enough to warrant reporting to their care team.
Previous research on remote monitoring during chemotherapy has shown benefits, but is largely based on short trials from a single site or country, making it difficult to draw wider conclusions. To address this evidence gap, a team of international researchers set out to evaluate the effects of remote monitoring of chemotherapy related side effects on symptom burden, supportive care needs, anxiety, work limitations, and quality of life. Their published findings can be accessed here.
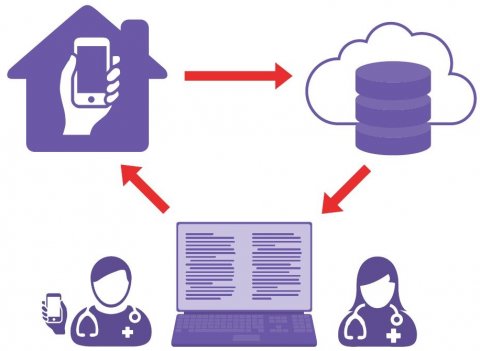
Image source: Maguire et al., BMJ 2021 (CC BY 4.0)
Their findings are based on 829 patients aged 18 years or older, diagnosed with breast cancer, colorectal cancer, Hodgkin’s disease, or non-Hodgkin’s lymphoma, and receiving chemotherapy at 12 cancer centres in Austria, Greece, Norway, the Republic of Ireland and the UK. Patients were randomly allocated to 24-hour symptom monitoring via the Advanced Symptom Management System (ASyMS) (intervention group) or standard care at their cancer centre (control group) over six cycles of chemotherapy. Intervention patients completed a daily symptom questionnaire on a handheld ASyMS device; this generated alerts to hospital clinicians if action was needed. Patients were also provided with self-care advice with information on how to manage their symptoms themselves.
The researchers found that for the intervention group, symptom burden remained at pre-chemotherapy treatment levels, whereas controls reported an increase from cycle 1 onwards. Analysis indicated significant reductions in favour of ASyMS for psychological and physical symptoms and for level of distress associated with each symptom. Health related quality of life scores were higher in the intervention group across all cycles, whereas average scores for anxiety were lower. Measures of cancer patients’ confidence and ability to engage in their care were also higher in the intervention group, and most supportive care needs were lower, including sexual related needs and physical and daily living needs. Other areas of supportive care needs and work limitations were similar in both groups, and the safety of ASyMS was satisfactory.
This is the largest trial to date of remote monitoring of symptoms during chemotherapy for cancers being treated with curative intent, and its robust design avoided many limitations of previous studies, say the researchers. They acknowledge some limitations, including technical problems and the fact that most participants had breast cancer and were female, suggesting a larger study is warranted for patients with other types of cancer. Nevertheless, they say their findings suggest that an evidence based remote monitoring intervention, such as ASyMS, has potential for implementation into routine care to make a meaningful difference to people with cancer. Remote monitoring systems will be vital for future services, particularly with blended models of care delivery arising from the Covid-19 pandemic, they add.
Source: BMJ
22.07.2021