Article • Reshaping GI cancer care
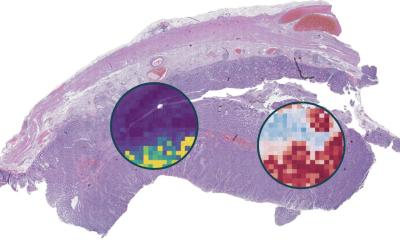
Pathologists at the heart of precision oncology
Biomarker testing is ushering in a novel era of therapy personalisation for gastroesophageal and colorectal cancers, according to experts presenting at the 37th European Congress of Pathology in Vienna this September. During a session on state-of-the-art in gastrointestinal biomarkers, speakers outlined how targeted therapies and immunotherapies are transforming treatment options – but emphasized that pathologists must remain at the center of this evolution.
By Mark Nicholls
© peterschreiber.media – stock.adobe.com
The session covered emerging biomarkers in metastatic and non-metastatic colorectal cancers, treatment considerations for esogastric cancers, new targeted therapies, and emerging detection techniques.
While biomarkers have 'opened the door to precision oncology,' challenges remain, particularly around detection accuracy, tumour heterogeneity, and the need for experienced interpretation. As one speaker noted, pathologists need to 'stay involved and engaged' to help shape how biomarkers are applied for patients' benefit.
From chemotherapy to precision targeting
Photo courtesy of Dr Shia
Jinru Shia, MD, from the Memorial Sloan Kettering Cancer Center in New York presented on emerging biomarkers in metastatic and non-metastatic colorectal cancers (CRCs), outlining the evolving landscape of biomarkers in this field.
She explained how systemic chemotherapy, long dominated by fluorouracil, expanded around the year 2000 with the introduction of irinotecan and oxaliplatin. These formed the familiar backbones of FOLFOX, FOLFIRI, and CAPEOX – regimens, she emphasized, that still underpin treatment today, but have since been joined by targeted therapies.
'Targeted therapy is where predictive biomarkers come in,' she said, highlighting how cetuximab's arrival in 2004 to target EGFR opened the door to a wave of additional agents, including those against VEGF, VEGFR2, NTRK fusions, HER2 amplification, BRAF V600E mutations, and now even KRAS G12C, 'long thought undruggable.'
Alongside targeted approaches, she said immunotherapy has brought dramatic change, describing the first FDA approval in this space – pembrolizumab in 2017 – as a watershed moment not just for colon cancer but as the first tissue-agnostic approval across solid tumours with mismatch repair (MMR) deficiency. More recently, immunotherapy has moved into earlier-stage settings.
Precious targets
Yet she cautioned that the proportion of colorectal cancers carrying actionable targets remains relatively small (15-20%) in the metastatic setting – with KRAS G12C, HER2, NTRK, and MMR deficiency each confined to small subsets. 'The targets are precious,' she said. 'And they are only as good as our ability to detect them.'
Dr Shia then examined detection via immunohistochemistry (IHC), focusing on strengths and pitfalls across specific biomarkers:
- NTRK fusions are extremely rare in CRC, with IHC useful as a screening tool but with a false-positive rate of around 20%, requiring RNA-based confirmation.
- BRAF V600E IHC generally correlates well with mutation status, though pitfalls include mucin-associated artifacts and heterogeneous staining.
- HER2 testing criteria for CRC adapt the HERACLES trial cut-off, but tumour heterogeneity can drive resistance to anti-HER2 therapy, as illustrated by relapse following initial response.
- MMR deficiency is, of all biomarkers, the most biologically complex.
'Intratumoral heterogeneity and subclonal loss can blunt response to checkpoint inhibitors, and MMR-deficient status does not always equate to MSI-high, particularly in non-colorectal tumours,' she told delegates.
These caveats, she suggested, show why the tissue-agnostic paradigm is not always straightforward. 'MMR deficiency across cancers is not uniform, and it may be MSI-high status that truly drives immunogenicity. Future efforts should aim for not only the most sensitive tests to detect MMR failure, but tests that predict response.'
Concluding, Dr Shia noted: 'The biomarker era has opened the door to precision oncology, bringing real impact to patient care. But challenges remain at the forefront, and pathologists need to stay engaged to help shape how biomarkers are applied for patients' benefit.'
Challenges of increasing complexity
Matteo Fassan, Professor of Pathology at the University of Padua in Italy, provided an overview of biomarker testing in gastroesophageal cancers, highlighting the essential role that preanalytical and analytical factors play in biomarker evaluation.
We are facing a novel era of therapy personalisation for gastroesophageal cancer and biomarkers are essential in guiding targeted treatment choice
Mateo Fassan
He discussed the 'core biomarker testing portfolio' of HER2, PD-L1, MMR/MSI, CLDN18.2 and, in the future, FGFR2b, though warned that in a situation that is becoming increasingly complex, preanalytical variables can interfere with biomarker evaluation. He also emphasized the importance of having an 'adequate number of biopsies for an adequate evaluation of the molecular landscape.'
Fassan explained that PD-L1 should be tested with 22C3, 28-8 or SP263 clones while CLDN18.2 expression is currently evaluated with the 43-14A clone. 'With the clinical/therapeutic impact of biomarker evaluation, there is a need for experienced GI pathologists for evaluation and they need to be at the centre of the patient journey,' he continued. 'We are facing a novel era of therapy personalisation for gastroesophageal cancer and biomarkers are essential in guiding targeted treatment choice.'
However, he said that biomarker evaluation is affected by several factors: an intrinsic heterogeneity due to preanalytical, analytical and evaluation variables; and biomarker expression/status can change over the course of the cancer disease and depend on the therapies carried out.
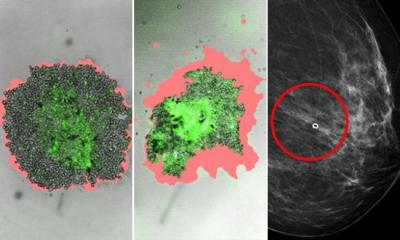
Speakers at the congress also highlighted the Trop-2 protein as a promising therapeutic target.

Photo courtesy of Dr de la Fouchardière
Dr Christelle de la Fouchardière from the medical oncology department at the Institut Paoli-Calmettes (IPC) in Marseille spoke on agnostically-developed targeted therapies in digestive cancers, colorectal cancers, esophagogastric adenocarcinomas and biliary tract carcinomas.
From traditionally targeted therapies of small molecules like tyrosine kinase inhibitors (TKIs) and large molecules like monoclonal antibodies (MABs), she said that with the new targeted therapies in 2025 the therapeutic landscape is far more extensive.
'We have several drugs that often combine cytotoxic drugs, targeting some cancer protein or bridging tumour and immune cells,' she said. 'In digestive cancers the most widely used are antibody drug conjugates and bispecific antibodies and we also have preliminary results with CAR T-cells but no such drug is yet approved in this setting.'
With new targeted therapies in digestive oncology emerging in the last decade, she said the 'new type of thinking' was 'mostly biomarker-driven rather than purely organ-based therapies.'
'Digestive oncology is entering the era of precision medicine. Pathologists and molecular biologists play a pivotal role in identifying the right target in the right patient at the right moment and multidisciplinary collaboration/discussion is essential,' de la Fouchardière concluded.
The session also heard from Rondell Graham, Professor of Laboratory Medicine & Pathology at Mayo Clinic in Minnesota, who discussed emerging techniques used to determine biomarkers and regulatory aspects of biomarker determination.
Profiles:
Jinru Shia, MD, is Member and Attending Pathologist at Memorial Sloan Kettering Cancer Center, Professor of Pathology and Laboratory Medicine at Weill Cornell Medicine and the director of the GI pathology service at MSKCC. Her primary clinical focus is GI, liver and pancreas pathology, and her main research interest centres on familial and sporadic colorectal cancers, including Lynch syndrome associated neoplasia.
Matteo Fassan is Professor of Pathology at the University of Padua and Chief of the molecular Pathology Diagnostics Unit of the Padua University Hospital with research focused on the histological and molecular characterisation of pre-neoplastic and neoplastic gastrointestinal pathology.
Dr Christelle de la Fouchardière has been a medical oncologist at the Institut Paoli-Calmettes in Marseille since April 2023, specialising in digestive cancers, especially gastric and esophageal cancer. She previously directed the digestive oncology unit at the Léon Bérard Center in Lyon.
27.10.2025