Photo: Mark Nicholls
Article • Coronavirus disease research
Seeking a COVID-19 antidote: the potential of ACE2
As coronavirus disease COVID-19 continues to jet and alight invisibly around the globe, scientists now report that the virus has mutated to become two strains: the older ‘S-type’ appears milder and less infectious, while the later-emerging ‘L-type’, is more aggressive, spreads more quickly, and currently accounts for about 70 per cent of cases.
Report: Mark Nicholls
Worldwide, medical researchers are exploring whether existing viral treatments just might work against the new strains as well as examining which current research should speed into trials. In Australia, researchers have reasoned that a well-known HIV drug could work against the new coronavirus, for example, whilst other reports indicate that Chinese scientists have seen success in delivering high intravenous doses of Vitamin C to seriously infected patients (The journal Caduceus also reports that large shipments of Vitamin C are now enroute to that country). Meanwhile, ACE2 raises hopes as a rational therapy against this devastating viral attack.
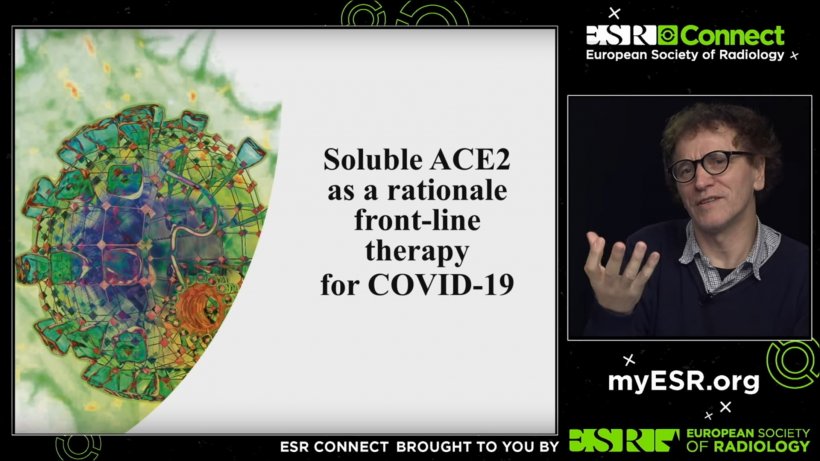
Scientific hopes are that the angiotensin converting enzyme 2 (ACE2) will play a critical role in tackling the COVID-19 pandemic. During a live webcast lecture ‘ACE2 – a rational frontline therapy for COVID-19’, organised by the European Society of Radiology, the enzyme’s background, development and potential role as a therapy was explored by one of the world’s leading geneticists and molecular immunologists.
The whole presentation can be viewed on YouTube:
Professor Josef Penninger outlined the relationship between ACE2 and the renin-angiotensin system (RAS) – responsible for systemic vascular resistance and for regulating blood pressure and fluid-electrolyte balance in instances of lung injury – highlighting the predisposition of ACE2 as a SARS-CoV and SARS-CoV-2 receptor and potential treatment approach.
If you knock out ACE2, disease gets much worse and if you have ACE2 it gets much milder because it counterbalances the ACE function and, by doing so, regulates the system
Josef Penninger
Starting more than two decades ago, the research led to the discovery of ACE2, initially in fly and mouse models and then indicating a human link and, the expert explained, how more recently that has led his team to believe they are closer to testing a medicine for COVID-19. From a knockout mouse model, they found that, if ACE2 was lacking then heart function was impaired, and was a negative regulator of the RAS. This also pointed to a possible gender bias in COVID-19 – with ACE2 on the X chromosome, meaning males have one copy and females two. ‘In simple terms,’ Penninger said, ‘ACE cleaves to amino acid from angiotensin 1 to make angiotensin 2, which acts on receptors 81 and 82. ACE2 is a catalytically active molecule on the surface of cells – though it can also be soluble in serum – and inactivates this pathway.’
From there, the research showed that ACE2 also affects kidney disease and regulates liver and lung fibrosis. ‘If you knock out ACE2,’ he continued, ‘disease gets much worse and if you have ACE2 it gets much milder because it counterbalances the ACE function and, by doing so, regulates the system.’ With a lack of ACE2 in the lung leading to severe injury, research by other groups in the early 2000s had indicated that ACE2 might be a receptor for the SARS coronavirus of 2003. With the explanation of SARS binding to ACE2 and enhancing disease severity, his team saw a new pathway to develop a medicine against acute lung injury. ‘Based on this, we decided to develop a human recombinant angiotensin renin converting enzyme for the therapy of lung injury,’ Penninger said.
He also highlighted the difference between the SARS virus of 2003, which infected about 8000 people leading to 800 deaths, and COVID-19. For SARS to spread, a patient had to be very ill and in close contact with other individuals to transmit, whereas the new virus is easy to transmit. ‘That’s why there is fundamental difference between old outbreak and new outbreak. What we believe is happening is that the virus comes in via this spike protein, binds to ACE2 and together with ACE2 gets into the cell, fuses to the membrane, the virus gets out from the endosome, and replicates. So, ACE2 is essential for binding to the virus and surface – of course this leads to viral release and replicates and then spread, leading to diseases we know as SARS and COVID-19.’
Recommended article

Interview • Chest X-ray, CT and more
Imaging the coronavirus disease COVID-19
Chest X-ray is the first imaging method to diagnose COVID-19 coronavirus infection in Spain, but in the light of new evidence this may change soon, according to Milagros Martí de Gracia, Vice President of the Spanish Society of Radiology (SERAM) and head of the emergency radiology unit at La Paz Hospital in Madrid, one of the hot spots for viral re-production of COVID-19.
Currently, Apeiron Biologics AG, a company founded by Penninger, is scheduled to start a pilot clinical trial for a newly-developed drug designed to decrease mortality in those affected by the virus. ‘This is where we believe our soluble ACE2 would come in,’ he explained, ‘Because ACE2 sits on the membrane and our molecule is soluble, it would soak up the virus like a neutralising antibody, so the virus cannot find its real receptor. With less virus coming, this would slow down viral infection and improve disease because the virus cannot properly get in and infect the cells. We believe, based on the discovery of ACE2 – and its function as a negative regulator of renin angiotensin, protecting heart, kidneys, liver, protecting the lung – this would make sense as a therapeutic for COVID-19.’
This, he concluded, would have two functions – taking the virus away from its real receptor by working as a neutralising antibody and, second, protecting tissues – as in the lung – from the disease. Penninger emphasised that carefully-designed placebo controlled trials in COVID patients are now needed to test the science.

Profile:
As one of the world’s leading geneticists and molecular immunologists, Professor Josef Penninger has gained numerous awards for his work and research and he is also author of around 1100 publications. He established the Viennese Institute of Molecular Biotechnology and is the current Director of the Life Sciences Institute at the University of British Columbia in Canada. The main focus of his work has been autoimmune, bone, and heart and lung diseases, and cancers.
18.03.2020