Interview • Chest X-ray, CT and more
Imaging the coronavirus disease COVID-19
Chest X-ray is the first imaging method to diagnose COVID-19 coronavirus infection in Spain, but in the light of new evidence this may change soon, according to Milagros Martí de Gracia, Vice President of the Spanish Society of Radiology (SERAM) and head of the emergency radiology unit at La Paz Hospital in Madrid, one of the hot spots for viral re-production of COVID-19.
Interview: Mélisande Rouger
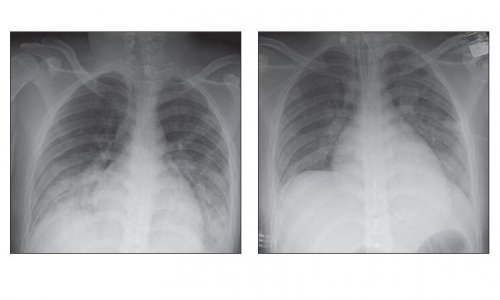
Image courtesy of Dr Martí de Gracia
HiE: How are you coping with the outbreak at your hospital?
Milagros Martí de Gracia: ‘We’ve been preparing for this situation for several days; the number of patients has grown progressively, and has surged this past couple of days. We now have 200 patients with confirmed COVID-19 coronavirus infection (as of March 12). Patients have been gradually placed in wards that can accommodate between 14 and 25 persons each. We have five wards dedicated exclusively to patients with suspected infection.
‘Naturally, this has had an impact on the organisation of the emergency radiology unit. Patients with very high suspicion and confirmed infection are examined with portable radiology equipment. Suspicious patients are examined in the emergency radiology room, which is currently exclusively dedicated to this purpose. Patients without suspected infection are waiting to be attended or are located in other wards. Radiological examinations are done in another area of the hospital, away from the main area, so that patients do not mix.’
HiE: How do these measures affect your department’s workflow?

MMG: ‘The request for chest radiographs has grown exponentially and proportionally with the number of patients visiting the emergency department. A chest X-ray is performed in suspected or confirmed patients through specific circuits. Rooms with dedicated equipment are allocated exclusively for possible patients. Portable radiology equipment is available for confirmed or suspected patients.
‘This is easier to organise when teams are dedicated exclusively to the emergency department, or when emergency radiology units are integrated in the emergency department.’
HiE: How many patients have you admitted so far?
MMG: ‘We attend more than 400 daily emergencies only in the general hospital. Every day we receive around 140 alerts. Today, on March 12, more than 200 patients have been confirmed with the virus, many of whom have already been admitted.
‘At first, the epidemiological criterion was the most important information, i.e. having travelled or contacted someone from China or Korea. Later the criterion was having had contact with someone infected or coming back from Italy. But now in Madrid, we only need to assess the symptoms, which are very nonspecific (cough, fever and respiratory distress). However, there may be other symptoms that complicate suspicion. Analytical alterations such as lymphopenia, elevation of transaminases or lactate dehydrogenase augment the degree of suspicion.’
HiE: What is the protocol?
This is a fast-evolving issue and today’s recommendations might not be valid tomorrow
Milagros Martí de Gracia
MMG: ‘Patients with respiratory symptoms must remain isolated and wear a mask. If clinical suspicion persists after the examination, a sample of nasopharyngeal exudate is taken to test reverse-transcription polymerase chain reaction (RT-PCR). Then, we perform a chest X-ray. Getting the results of the PCR test may take several hours. The chest X-ray is a discriminating element; if the clinical situation and the chest X-ray film are normal, patients can go home and wait for the results of the etiological test. But if the film shows pathological findings, patients are admitted to the hospital for observation.
‘Usually the absence or presence of pathological findings on chest X-ray is determining to send the patient home or keep him/her under observation But if the clinical suspicion is high and the PCR or/and chest X-ray is normal, a chest CT is indicated.
‘This is a fast-evolving issue and today’s recommendations might not be valid tomorrow. The SERAM is developing and updating guidelines for radiologists that are available on our website. We have also created working groups to help not only diagnose the virus, but also to promote safe management among patients and healthcare staff.’
HiE: How important is radiology in diagnosing COVID-19 infection?
MMG: ‘Radiology is fundamental in this process. The radiologist's main contribution is to facilitate and expedite as much as possible the exploration, help design specific circuits and provide a fast and accurate report of the radiological findings that should indicate whether or not these are consistent with the COVID-19 coronavirus infection.’
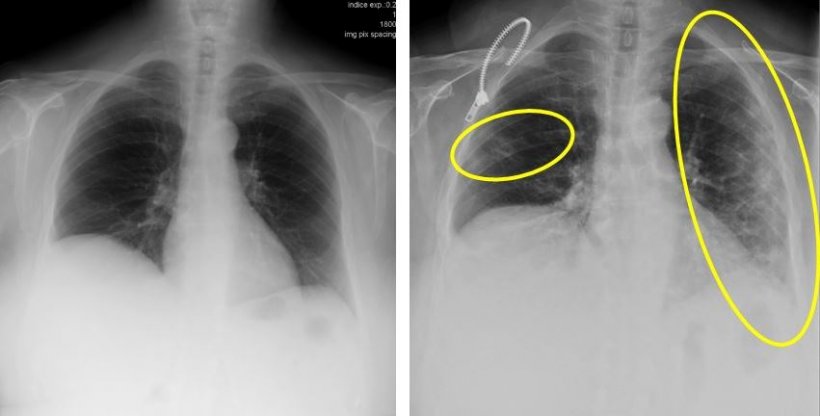
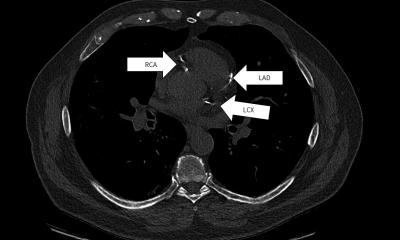
Images courtesy of Dr Martí de Gracia
HiE: What are the typical radiological findings?
MMG: ‘The findings that make us strongly suspect that we are dealing with a COVID-19 infection are the ground glass patterned areas, which, even in the initial stages, affect both lungs, in particular the lower lobes, and especially the posterior segments, with a fundamentally peripheral and subpleural distribution. These findings are present on chest CT in practically 50% of patients in the first two days; For this, in China, CT is being used as a screening or diagnostic method.
‘These lesions progress in the following days until they become more diffuse. If they associate with septal thickening, they will present with a crazy paving pattern. In general, they progress in extension and also towards the consolidation that is done concomitantly with the ground glass pattern, which can present a rounded morphology. It is very rare that it associates lymphadenopathy or capitation or pneumothorax, as the Middle East respiratory syndrome coronavirus (MERS-CoV) did.’
Recommended article

Article • MERS-CoV
Seeking answers to combat Middle East respiratory syndrome
With a case fatality rate of 35 percent, a Middle East respiratory syndrome-related coronavirus (MERS-CoV) infection – also called camel flu – is a dangerous disease. About seven years ago, when the virus was first isolated, mortality was close to 100 percent since only severe infections that led to the patient being in intensive care were recorded. Today the environment of each victim is…
HiE: Do you also use imaging to follow-up the disease?
MMG: ‘We have had little time to discuss our experience in the follow-up of infected patients so far. But, for the time being, radiology is playing a crucial role in the diagnosis and identification of patients for observation in the hospital admission or at home. The most commonly used diagnostic modality is chest radiography. At the moment, computed tomography (CT) plays a limited role and is carried out in cases of clinical mismatch and PCR, i.e. in patients with high suspicion of being infected but with negative or inconclusive PCR. CT is also indicated for the recognition of possible complications that are not obvious on the chest radiograph, or to diagnose very serious patients quickly, whose PCR results are not yet available, for placement in a specific coronavirus intensive surveillance unit.
‘In other countries like China, CT is being used as a diagnostic modality because of its high sensitivity to show lung lesions before PCR. The WHO considers typical CT findings as a diagnostic criterion since February 17. We have published our recommendations on our website https://www.seram.es, and will update them soon.’
Recommended article

News • COVID-19 in radiology
CT outperforms lab diagnosis for coronavirus infection
In a study of more than 1,000 patients published in Radiology, chest CT outperformed lab testing in the diagnosis of 2019 novel coronavirus disease (COVID-19). Researchers at Tongji Hospital in Wuhan, China, concluded that CT should be used as the primary screening tool for COVID-19. In the absence of specific therapeutic drugs or vaccines for COVID-19, it is essential to detect the disease at an…
HiE: After a decade of healthcare budget cuts in Spain, do you have enough equipment to face the outbreak?
MMG: ‘Certainly the high number of infected is a great challenge for public health in Madrid and Spain because we have suffered great cuts due to the crisis. In my department, a priori, we did not have enough equipment to face the crisis but agreements have been reached for its immediate acquisition of several digital portable equipment for the radiology department and mechanical ventilation equipment for the ICUs.’
HiE: Really, how dangerous is COVID-19?
MMG: ‘It has been compared a lot with ‘flu, but really the only thing it has in common is that it is transmitted through the flow drops and by contact. COVID-19 is much more contagious; unlike the flu, there is no vaccine and for our immune system it is an absolute unknown because we have never been in contact with it.’
HiE: What do you think of the response of Madrid’s authorities to this virus spread?
It’s very difficult when decisions have such important economic repercussions. But people's health is the most important
Milagros Martí de Gracia
MMG: ‘It‘s certainly very difficult to make decisions and choose the right time to minimise impact, knowing that you have to make these decisions as soon as possible. It’s very difficult when decisions have such important economic repercussions. But people's health is the most important.’
HiE: The UK has called back retired physicians to help. Could this be a viable strategy for Madrid?
MMG: ‘Here, now, emergencies need support and reinforcement, which can be offered by doctors from other specialties inside the hospital. I don’t know if the possibility of calling retired doctors is being considered, but numerous doctors and nurses have been hired to reinforce guards in strategic places, such as intensive microbiology and emergencies.’
HiE: Have we just seen the tip of the iceberg? What are the projections for the next few weeks or months?
MMG: ‘From what I’ve read, COVID-19 shares many characteristics similar to SARS and MERS. So, we all believe that the beginning of the ‘hot’ season will actually reduce the transmission capacity of the virus, and it becomes a seasonal virus.’
HiE: What do you recommend to fellow radiologists?
MMG: ‘I encourage all my fellow radiologists to participate actively in the protocols of action within the hospital and provide what radiologists do best: the radiological report. That is our most important added value.
‘The epidemic is still in the ascending phase, and it’s very likely that it will not stabilise until the next few weeks. That’s why containment measures are so important: we know that a large part of the population is going to be infected but it is essential that this contagion is made in a staggered way, with a curve as flat and slow as possible to avoid the collapse of the healthcare system.’
Profile:
Milagros Martí de Gracia is Vice President of the Spanish Society of Radiology (SERAM), President of the Spanish Society of Emergency Radiology (SERAU) and head of the department of emergency radiology at La Paz Hospital, a general tertiary hospital in Madrid. She was President of La Paz’s Catastrophe Committee from 2006 to 2019 and is now its Vice President. She is a founding member of the European Society of Emergency Radiology (ESER). A graduate from the Complutense University she gained her MD from the Autonomous University in Madrid, where she is Honorary Professor of Medicine.
16.03.2020