Article • Modality comparison
COVID-19 imaging: lung ultrasound vs chest CT
A recent preprint study in France underpins the debate on whether lung ultrasound (LUS) should be used to triage COVID-19 patients better at the hospital as well as in primary care.
Report: Mélisande Rouger
The eChoVid study, published as a preliminary report of work on medRxiv, shows that LUS enables identification of lung lesions as well as chest CT in COVID-19 patients. A team of French researchers compared routinely collected data in 107 patients in three emergency units of Assistance Publique des Hôpitaux de Paris (APHP) who underwent LUS, a short clinical assessment by two emergency physicians blinded to each other’s exams and a CT examination, between 19 March and 1st April 2020.
Recommended article

Interview • Chest X-ray, CT and more
Imaging the coronavirus disease COVID-19
Chest X-ray is the first imaging method to diagnose COVID-19 coronavirus infection in Spain, but in the light of new evidence this may change soon, according to Milagros Martí de Gracia, Vice President of the Spanish Society of Radiology (SERAM) and head of the emergency radiology unit at La Paz Hospital in Madrid, one of the hot spots for viral re-production of COVID-19.
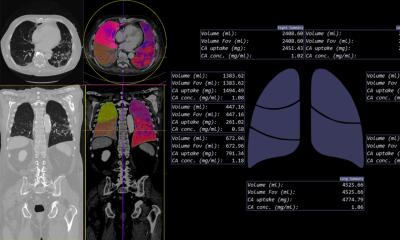
Researchers defined a severity global score ranging from 0 to 24, with LUS consisting of scoring lesions in eight chest zones from 0 to 3 and a CT severity score ranging from 0 to 3, according to the extent of interstitial pneumonia signs. 48 patients underwent LUS by both an expert and a newly trained physician. The authors found that LUS’s global score showed good performance to predict CT severity assessment of COVID-19 as normal versus pathologic, with 95% sensitivity and 83% specificity. Similar performance was found for CT assessment, as normal or minimal versus moderate or severe, with 86% sensitivity and 78% specificity.

Good agreement was also found for zone scoring assessed by a new trainee (30mn theory + 30mn practice) and expert; moderate agreement was found for new trainees and experts. ‘The global score is a simple tool to assess lung damage severity in patients with suspected or diagnosed COVID-19. Comparing the performance of new trainees and expert physicians opens a path for the adoption beyond the scope of experts. LUS is a good candidate for patients triage, especially in case of CT availability issues,” the authors concluded.
These results suggest that ultrasound could help pre-identify and triage patients in the emergency unit before they undergo CT, regardless of the readers’ experience, according to Lucie Beylacq, anaesthesiologist/intensivist at Thiers Clinic in Bordeaux and CEO of medTandem, a company that promotes online peer-to-peer training.
‘The study confirmed something we long suspected: that LUS can help triage patients before CT. LUS could be very useful to identify those patients with lung lesions, but no clinical sign, who are typically sent home and must be admitted in the emergency unit five to seven days later,’ Beylacq explained. The global score, combined with clinical correlation and PCR results, will offer a more panoramic vision of the patient’s clinical condition, she added.
A controversial tool in France
The report highlights the controversial role of ultrasound in France, where the National Authority for Health (Haute Autorité de Santé, HAS) has excluded LUS in its recommendations on how to image COVID-19. The HAS reportedly acted on a publication issued by the French Society of Radiology (Société française de Radiologie, SFR), which does not endorse the technique for the assessment of confirmed or suspected patients. Chest CT is currently used as the reference for assessing pulmonary injury in suspected or diagnosed COVID-19 with signs of clinical severity.
The echoVid report doesn’t question the role of CT and PCR in diagnosing COVID-19, but suggests that LUS could help quickly in assessing lung status in these patients and save time in primary care and at the hospital, according to Beylacq. ‘LUS is quicker, cheaper, more available and easier to perform for emergency physicians, general practitioners or intensivists, who are already in contact with patients,’ she pointed out.
Despite the HAS recommendations, a number of intensivists, emergency physicians and general practitioners have used LUS to manage COVID-19 in France, she added. ‘I’ve had a lot of feedback from colleagues, especially in the East, one of the most affected areas in the country, on how they’ve used LUS to handle patients,’ Beylacq said.
Recommended article

Article • Coronavirus in radiology
Why we need a global view of COVID-19
There are major complications from COVID-19 – ARDS, pulmonary embolism and neurological – that imaging can help detect, manage and/or follow up in the long term, radiologists from France and the UK explained during a recent ESR Connect session. ARDS is the most dreaded complication and the number one morbidity in COVID-19 patients. The incidence was up to 30% of patients in initial reports.…
LUS is also performed in other European countries by emergency physicians for triage and by intensivists for patient management. Ventilation pioneer Luciano Gattinoni, from the Department of Anaesthesiology and Intensive Care at Medical University of Göttingen, Germany, highlighted the role of LUS in a study last April, in which he defined two groups: patients with anterior/posterior interstitial lesions and patients with condensations/mainly posterior lesions. This classification is considered a strong indicator of the ventilation technique to be used – PEEP or prone position. At Murcia Quiron Salud Hospital in Spain, anaesthesiologist Vicente Roquès Escolar and team have also used LUS in their patients, after recommendations shared by colleagues in Madrid.
LUS is part of basic training for intensivists and emergency physicians in a number of scenarios such as pleural effusion, pneumothorax, respiratory distress, etc. Intensivists are used to looking at the interstitial syndrome to adapt ventilation, and could use their skills in COVID-19 management. General practitioners could also easily learn how to use LUS to help diagnose and triage patients, Beylacq believes. ‘Any physician can learn how to use LUS very quickly,’ Beylacq concluded. ‘It only takes 30 minutes in the study and five patients imaging with a mentor. medtandem.com organised a free video and videoconference every three days to help all our colleagues to learn and share information about LUS and COVID-19,’
23.09.2020