Article • MRI vs. Alzheimer's
Seeking leaks in the blood-brain barrier
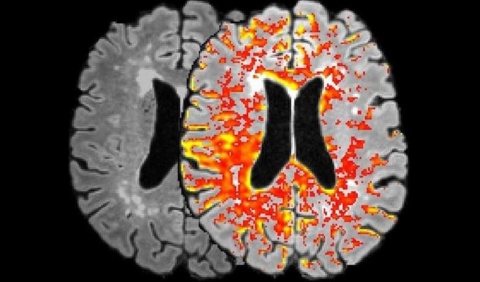
‘With our new MRI method, we can finally visualise tiny leaks in the blood-brain barrier. They shed light on the vascular contribution to dementia and may indicate Alzheimer’s disease. However, the MRI scan is only a tool to diagnose cerebrovascular damage. We have not yet found a cure for Alzheimer’s,’ confirms Walter H Backes, medical physicist and professor at Maastricht University Medical Centre.
Report: Madeleine van de Wouw
The blood-brain barrier (BBB) separates blood from the brain tissue and protects the brain by allowing certain substances to pass while keeping others out. Backes, with his interdisciplinary team of Maastricht UMC and Leiden UMC, are hot on the tracks of Alzheimer’s disease (AD) as they aim to visualise small vessel leakage in BBB.
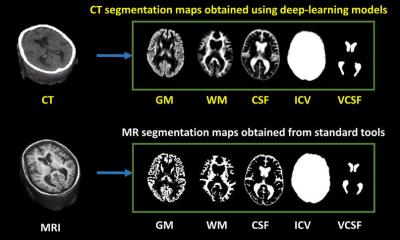
Contrast-enhanced MRI

While conventional MRI visualises neither small vessels nor markers or leakage, the dynamic scan traces even extremely low concentrations of the marker fluid everywhere through the bloodstream and brain tissues, no matter how small the vessels are. ‘Contrast-enhanced MRI is a combination of vision, technical knowledge and computer power,’ says Backes, adding: ‘We now can investigate with medical imaging in a non-invasive way and we don’t have to rely on post-mortem tissue or spinal tap samples anymore.’ Initial clinical tests yielded exciting insights: ‘Since we couldn’t test our new scanning method in healthy volunteers with an intact BBB we immediately scanned Alzheimer patients and saw damages in the barrier with fluid leaking from the smallest blood vessels to the brain.’
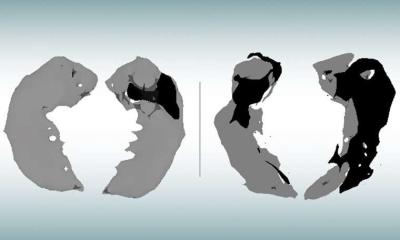
New insights in the vascular contribution of dementia
Due to the leakage, unwanted substances can enter the brain and damage the tissue. ‘At first, blood vessels were not considered a player in the development of AD. While animal experiments had shown leaking blood vessels, these leaks were not thought to be associated with cognitive decline and dementia. What we discovered in the human brain is somewhat of a fluke, an accidental breakthrough. While we can show the leak, we cannot determine yet whether it is AD. This requires further research. Nevertheless, the connection between BBB impairment and AD pathology was strengthened by the fact that the addition of diabetes and other non-cerebral vascular diseases did not change the results.’
The condition of the blood vessel system, Backes concludes, seems to play a very important – and previously underestimated – role in the development of Alzheimer’s disease. ‘Earlier research focused the deposition of amyloid-beta proteins as a possible cause of AD. This theory appears to be disproven today: When we wipe out the protein stack with medication, the condition of the patient remains unchanged. Finding this leakage is therefore an important contribution to the research on the development of AD. We have shown that in people with Alzheimer’s disease not only the brain but also blood vessels are damaged, and that the damage is substantial.’
While there is no cure yet for Alzheimer’s, Backes’ research might indicate that keeping our vascular system in good condition – with good nutrition and physical as well as mental exercise – could help stave off AD.
In eight years we should have a better understanding of the cause of Alzheimer’s
Walter H Backes
Unfortunately, the new MRI method is not yet widely available. Therefore, as the physicist explains, ‘We are focusing on making the technique easier to apply, so more people can be examined, even those who do not yet show symptoms. With our new knowledge of the leaks, we might be able to send medication to certain places in the brain. However, we don’t yet exactly know how vascular medication works in vascular disorders. This will need further investigation.’ Indeed, two follow-up studies are planned, each lasting about four years. Backes: ‘In eight years we should have a better understanding of the cause of Alzheimer’s. Approximately one hundred people with and without diagnosed AD will participate in each trial.’
Award-winning research
During RSNA 2017, the article Backes and his team published in ‘Radiology’* received the Alexander R Margulis Award for the best scientific article of the past year. For Backes the award did not come as a surprise because his research had attracted considerable attention: ‘It feels very special to get the prize as a physicist. I am not a physician, not a radiologist. It is certainly an incentive to continue. The jury thought it was a provocative investigation that breaks with the current view that blood vessels play no role in the Alzheimer’s process.’
So where is AD research heading? ‘Since the BBB not only allows nutrients but also medication to pass’, Backes explains, ‘we might be looking at opening the BBB with sound waves and thus administering medication locally. Many questions remain to be answered: in the event of a leak, the liquid seeps through everything, but how will that work when we open the barrier artificially. Will the opening close again? Will such a procedure improve the quality of life? Can we possibly administer medication indirectly? In short, the possibility to visualise the leak in the blood-brain barrier opens many doors for all kinds of new research. There is still a lot to be done and even more to be expected.’
*http://pubs.rsna.org/doi/10.1148/radiol.2016152244
Profile:
Medical physicist Walter H Backes is professor at Maastricht University Medical Centre in the Netherlands, where his research focuses on magnetic resonance imaging of neurological and vascular diseases. In 1999, he established functional imaging of brain diseases for research and clinical examinations. Since then his imaging research expanded to include oncology, vascular and neurologic applications. Currently, his research examines novel imaging techniques, including (contrast-enhanced) angiography, perfusion and diffusion imaging and functional MRI of brain networks in diabetes, epilepsy, Alzheimer’s and small-vessel disease. He initiated and supervises a certified post-academic training program in medical physics and lectures on various radiological imaging topics.
27.02.2018