© angellodeco – stock.adobe.com
News • Preventive blood test
Prostate cancer screening: Study advocates 5-year-interval
A simple blood test every five years is sufficient to screen low risk men for prostate cancer, new research has shown.
The PSA blood test checks the level of prostate-specific antigen, a marker for prostate cancer. In Europe, only Lithuania routinely screens men for prostate cancer based on their PSA levels, as the test has historically been seen as insufficiently reliable. The German study, presented at the European Association of Urology (EAU) Congress in Paris, involved over 12,500 men aged between 45-50 taking part in the ongoing PROBASE trial, which is testing different prostate cancer screening protocols. The research has also been accepted for publication in European Urology.
Our study is still underway, and we may find that an even longer screening interval, of seven, eight or even ten years, is possible without additional risk
Peter Albers
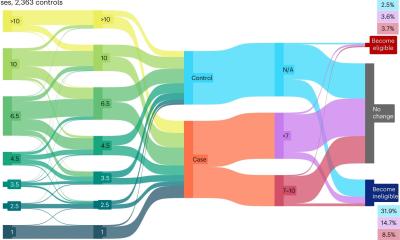
PROBASE is recruiting men aged 45 and splitting them into three groups based on their initial PSA test. Men with a PSA level of under 1.5 nanograms per millilitre (ng/ml) are deemed low risk and followed up with a second test after five years. Men with a PSA level between 1.5-3 ng/ml are deemed intermediate risk and followed up in two years. Those with a PSA level over 3 ng/ml are seen as high risk and given an MRI scan and biopsy.
Of over 20,000 men recruited to the trial and deemed low risk, 12,517 have now had their second PSA test at age 50. The researchers found that only 1.2% of these (146 in total) had high levels of PSA (over 3 ng/ml) and were referred for an MRI and biopsy. Only 16 of these men were subsequently found to have cancer – just 0.13% of the total cohort.
The EAU recommends that men should be offered a risk-adapted strategy (based on initial PSA level), with follow-up intervals of 2 years for those initially at risk, in which they include men with PSA over 1 ng/ml. The new findings suggest that the screening interval for those at low risk could be much longer with minimal additional risk.
Lead researcher, Professor Peter Albers, from the Department of Urology at Heinrich-Heine University Düsseldorf, explained: “By raising the bar for low risk from 1 ng/ml to 1.5, we enabled 20% more men within our cohort to have a longer gap between tests and very few contracted cancer in that time. With nearly 14 million men aged between 45-50 in Europe, the numbers affected by such a change would be significant. Our study is still underway, and we may find that an even longer screening interval, of seven, eight or even ten years, is possible without additional risk.”
Recommended article

Article • Research, diagnostics, therapy
Focus on prostate cancer
Prostate cancer (PCa) is not only one of the most common, but also one of the deadliest types of cancer in men. Diagnostics are correspondingly sophisticated, from imaging via ultrasound or MRI to various biopsy techniques – often even in combination. Keep reading for current developments in early detection, staging, therapy and research.
Prostate cancer screening has historically been a controversial subject, with concerns raised both around false positives leading to unnecessary invasive treatments and false negatives leading to cancers being missed. This is gradually changing due to MRI scans which can avoid unnecessary biopsies and the use of ‘active surveillance’, where men with early-stage cancer are monitored and only undergo treatment if their disease progresses.
The NICE guidelines here in the UK are incongruous. They say there’s no evidence that PSA screening is worthwhile, but at the same time say any man can ask for a PSA test if they want it
Phillip Cornford
Current guidelines and policies from European governments and health bodies remain contradictory and unclear, leading to high levels of opportunistic testing and inequality of access to early diagnosis, according to further research presented at the EAU Congress. The study reviewed early detection policies across the European Union and carried out focus groups with urologists to identify how guidelines were interpreted in clinical practice.
Dr Katharina Beyer, from the Department of Urology at the Erasmus MC Cancer Institute in Rotterdam, Netherlands carried out the research. She said: “Some country’s guidelines are actively against screening, others are non-committal and a few, such as Lithuania, have some form of screening. But in many countries, if you ask for a test, you can get one, sometimes free and sometimes not. This means that well-educated men, who know about PSA tests are more likely to be screened and get an early diagnosis, while others with less knowledge are at a disadvantage.”
This is also the situation in the UK, according to Professor Phillip Cornford, from Liverpool University Hospitals NHS Trust, who chairs the EAU Prostate Cancer Guidelines Committee. Professor Cornford said: “The NICE guidelines here in the UK are incongruous. They say there’s no evidence that PSA screening is worthwhile, but at the same time say any man can ask for a PSA test if they want it. The result is that well-educated, driven men ask and others, including many Afro-Caribbean men who are actually at higher risk, don’t ask and so prostate cancers get missed. There is clearly a need for more organised prostate cancer screening and last November, the UK government and the charity, Prostate UK, announced a £42m research programme to look at this. The details of that should soon be made public. Each country will need to design a screening programme that fits their health system and the resources they have available. But there is still plenty we can learn from other countries and the work underway in the EU. New findings, such as those from the PROBASE trial, can help us design an appropriate screening programme both in the UK and elsewhere.”
Source: European Association of Urology
07.04.2024