Oncology
Pancreatic cancer: Enzyme renders tumors resistant
Scientists at the German Cancer Research Center (DKFZ) and the Stem Cell Institute HI-STEM in Heidelberg have discovered the reason why some pancreatic tumors are so resistant to treatment. They have found that these tumor cells produce larger quantities of an enzyme that usually occurs in the liver and degrades many drugs. If this enzyme is blocked, the cancer cells become sensitive towards treatment again. The scientists have also been able to develop a test suitable for clinical use which is able to detect three different tumor types with varying disease progression.
Patients suffering from pancreatic cancer are often faced with a dismal prognosis: Once diagnosed, they may only have a few months left to live. This is mostly due to the late discovery of the disease, when the tumor has already metastasized. An operation at this point may no longer make sense. In addition, many tumors are resistant to chemotherapy.
We already know that there are three types of pancreatic cancer. A team of scientists around Andreas Trumpp and Martin Sprick from DKFZ and the Stem Cell Institute HI-STEM gGmbH, a partner of the DKFZ and the Dietmar Hopp Foundation, have gone further and have recently discovered that these three types differ not only in their aggressiveness, but also in their responsiveness to drugs.
The scientists found that the cells of the resistant subtype produce large quantities of the enzyme CYP3A5, which is normally active in the liver. First author Elisa Noll explains that 'the pancreatic tumor cells use this enzyme cascade to degrade drugs before they even get a chance to work. This makes them resistant to many of the cancer drugs currently used.' Martin Sprick adds 'We have already managed to block the enzyme both within the tumor cells and even in tumor-bearing mice, and to render the cells responsive to drugs again. We now hope to find a way to use this for patients as well.'
The drug-resistance caused by CYP3A5 can also occur during the course of the treatment. 'Around 20% of pancreatic tumors are drug-resistant from the outset due to the production of this enzyme. We expect however, that secondary resistance plays a role in even more patients,' says Sprick. The basis for this theory is that if the drug Paclitaxel is given for a prolonged period of time, tumor cells that were initially responsive start producing increased quantities of CYP3A5 and consequently stop responding to the therapy.
The scientists also found indications for a CYP3A5-caused drug resistance in other tumors such as gastric carcinoma and liver cancer. This previously unknown mechanism may also be responsible for the failure of individual clinical trials. The group now wants to investigate this in cooperation with the National Center for Tumor Diseases (NCT), a joint facility of the DKFZ and Heidelberg University Hospital.
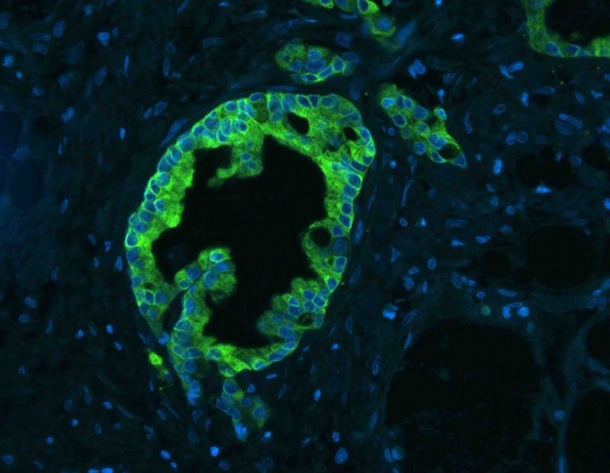
In order to establish whether a patient has contracted primarily resistant pancreatic carcinoma, scientists have also developed diagnostic markers. In cooperation with the European Pancreas Centre and the Institute of Pathology at Heidelberg University Hospital, they investigated the molecular structure of a large number of pancreatic tumors. Depending on the tumor subtype, the cultured cell lines from these tumors either produced KRT81 or HNF1A protein, or neither of them. With antibody staining, scientists are now able to identify these markers in patient samples quickly and reliably.
Literature:
Elisa M Noll, Christian Eisen, Albrecht Stenzinger, Elisa Espinet, Alexander Muckenhuber, Corinna Klein, Vanessa Vogel, Bernd Klaus, Wiebke Nadler, Christoph Rösli, Christian Lutz, Michael Kulke, Jan Engelhardt, Franziska M Zickgraf, Octavio Espinosa, Matthias Schlesner, Xiaoqi Jiang, Annette Kopp-Schneider, Peter Neuhaus, Marcus Bahra, Bruno V Sinn, Roland Eils, Nathalia A Giese, Thilo Hackert, Oliver Strobel, Jens Werner, Markus W Büchler, Wilko Weichert, Andreas Trumpp & Martin R Sprick: CYP3A5 mediates basal and acquired therapy resistance in different subtypes of pancreatic ductal adenocarcinoma, Nature Medicine 2016, doi:10.1038/nm.4038
Source: German Cancer Research Center
25.02.2016