News • New imaging agent
HER2-positive breast cancer: Whole-body PET/CT predicts targeted therapy response
A new imaging agent can predict early metabolic response to HER2-targeted treatment in metastatic breast cancer patients, according to new research.
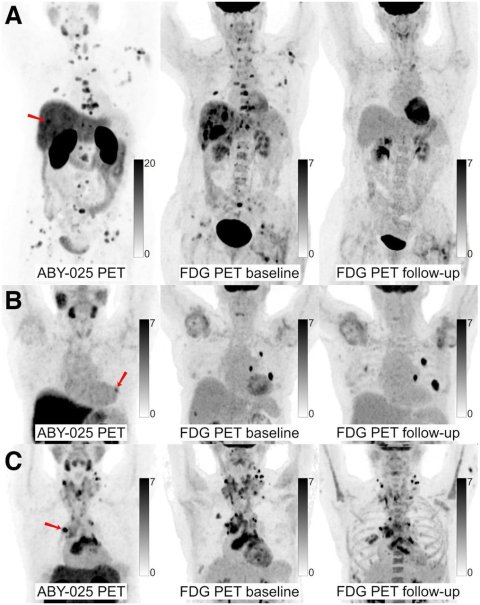
68Ga-ABY-025 PET/CT and 18F-FDG PET/CT images at baseline with 18F-FDG PET/CT follow-up after 2 cycles of treatment in biopsy-confirmed HER2-positive disease. (A) Patient with high 68Ga-ABY-025 uptake (SUVmax, 21) who previously received 3 lines of treatment. 18F-FDG PET/CT follow-up showed complete metabolic response. (B) Patient with low uptake (SUVmax, 5.4) who previously received 3 lines of treatment. 18F-FDG PET/CT follow-up showed disease progression (Δ-TLG, +68%) despite HER2-targeted treatment. (C) Patient with heterogeneous 68Ga-ABY-025 uptake who previously received 7 lines of treatment. 18F-FDG PET/CT follow-up showed heterogeneous response, with lesions higher in 68Ga-ABY-025 uptake tending to have better response. Arrows indicate biopsy sites.
Image source: Alhuseinalkhudhur et al., Journal of Nuclear Medicine 2023 (CC BY 4.0)
The results were published in the Journal of Nuclear Medicine. By providing whole-body quantification of HER2 expression, the new imaging agent, 68Ga-ABY-025 PET/CT, can play a valuable role in treatment planning and could spare patients from unnecessary drug-related side effects.
Up to 20% of breast cancer patients have HER2 overexpression, making HER2 an attractive therapy target for both new and recurring cases. However, since breast cancer is a heterogeneous disease and HER2 expression may vary within the same patient and over time, HER2-targeted treatment failure is common, and cure remains rare in metastatic disease.
“While HER2 status can be confirmed by biopsy results in early-stage breast cancer, it is more complicated in advanced disease where multiple metastases might have a heterogeneous HER2 expression,” said Ali Alhuseinalkhudhur, MD, PhD candidate in the Department of Immunology, Genetics, and Pathology at Uppsala University in Uppsala, Sweden. “Imaging the entire body rather than just the primary cancer site can give physicians a total estimate of HER2 expression so they can plan targeted therapies appropriately.”
Researchers investigated 68Ga-ABY-025 PET as a noninvasive tool for whole-body HER2-receptor quantification. Forty patients with known positive HER2 status were included in the study: 19 with primary breast cancer and 21 with metastatic breast cancer (median of three previous treatments).
A PET-based approach to evaluate the appropriateness of targeted therapy might help avoid unnecessary side effects and might provide a more personalized opportunity for timely therapy corrections
Ali Alhuseinalkhudhur
68Ga-ABY-025 PET/CT, 18F-FDG PET/CT, and core-needle biopsies from targeted lesions were performed at the baseline for each patient. 18F-FDG PET/CT was repeated after two cycles of therapy to calculate the directional change in tumor lesion glycolysis. Tracer uptake was measured in up to five of the largest lesions per patient, including the biopsied lesion. Standardized uptake values from 68Ga-ABY-025 PET/CT were then compared with the biopsied HER2 status and change in tumor lesion glycolysis.
68Ga-ABY-025 PET/CT successfully enabled quantification of HER2 expression, and uptake correlated significantly with metabolic response among patients, particularly in those with metastatic breast cancer. Also, an inverse association was found between the number of previous treatments and the metabolic response to the current treatment; the more treatments received, the higher the 68Ga-ABY-025 required to induce a metabolic response.
“The ability of 68Ga-ABY-025 PET/CT to provide a whole-body visualization of HER2 expression and to predict metabolic response is advantageous and exceeded the biopsy-based approach for metastatic breast cancer patients,” noted Alhuseinalkhudhur. “HER2-based imaging tools might provide a solution in situations where biopsies cannot be performed safely or when biopsy results are inconsistent. In addition, a PET-based approach to evaluate the appropriateness of targeted therapy might help avoid unnecessary side effects and might provide a more personalized opportunity for timely therapy corrections.”
He continued, “Our work is a strong example of the development toward personalized medicine. We hope that the value of quantification of biomarkers such as HER2 expression in cancer patients will be appreciated to a larger extent and introduced into nuclear medicine practice for both diagnostic imaging and therapy.”
Source: Society of Nuclear Medicine and Molecular Imaging
03.10.2023