Article • Radioembolization
Breast cancer metastasis: benefits and limitations of trans-arterial therapy
Evidence that radioembolization, a trans-arterial therapy, is safe and stops disease progression in metastatic breast cancer is increasing, a prominent American interventional radiologist showed at the Spectrum conference in Miami.
Report: Mélisande Rouger

Image source: Northwestern Medicine
It is common for patients with breast cancer to develop metastasis, according to Robert Lewandowski, MD, a professor of vascular and interventional radiology, medicine and surgery at Northwestern University in Chicago, US. ‘Over 50% of patients develop liver metastasis, which worsens prognosis,’ he said. ‘While 6 to 7% of patients have liver-only disease, less than 1% are candidates for surgical resection.’ The development of additional metastases, such as in the brain, is the cause of mortality in many patients who have metastatic breast cancer, he added.
Impact on liver function
Minimally invasive procedures are increasingly offered as an alternative or complementary to chemotherapy or hormonal therapy, but they may come at a cost. ‘Image-guided cancer therapies are impactful and expanding in application for patients with metastatic breast cancer,’ Lewandowski said. ‘However, these therapies can impact liver function, so this has to be considered when deciding which patients are best candidates for local therapies.’ Image-guided intra-arterial cancer therapies have been traditionally employed in the salvage setting, in patients with liver-only disease and limited to no systemic treatment options. These treatments are also an option in patients with stable limited extra hepatic disease and progression of hepatic tumours. ‘The goal is to control hepatic disease burden while preserving liver function,’ he said. ‘The other objective is tumour debulking and pain palliation from large hepatic masses.’
It is still unclear the impact image-guided cancer therapies, such as radioembolization, have on overall survival. ‘We still haven’t been able to show whether tumour control correlates with overall survival improvement,’ the expert said. ‘It’s complicated to evaluate what kind of a clinical impact we have on overall survival.’ A recent systemic review1 showed that radioembolization conferred control of tumour growth rate in most patients. However, its effect on patient survival needed to be elucidated further, the authors concluded.
A safe and efficient procedure
Lewandowski and colleagues conducted a study in 2014 that showed that radioembolization stopped progression of breast cancer liver metastases after failed chemotherapy.2 Glass microsphere radioembolization proved safe in a heavily pre-treated population with multi-focal liver metastases. ‘In our study, we treated 75 patients with metastatic breast cancer. 85% had multiple liver tumours and 77% had extra hepatic disease at the time of radioembolization, including 13% who had brain disease,’ he said, highlighting the collaborative approach required to care for these patients.
Most patients in the trial had been treated with chemotherapy or hormonal therapy before they underwent radioembolization. ‘There was an objective decrease in tumour size in 82% of patients after the procedure,’ said Lewandowski, who shared the images of a 54-year-old patient treated concomitantly with an oral chemotherapy agent and radioembolization. ‘The tumour reduced by over 50% on the next first follow-up scan one month after treatment onset,’ he said.
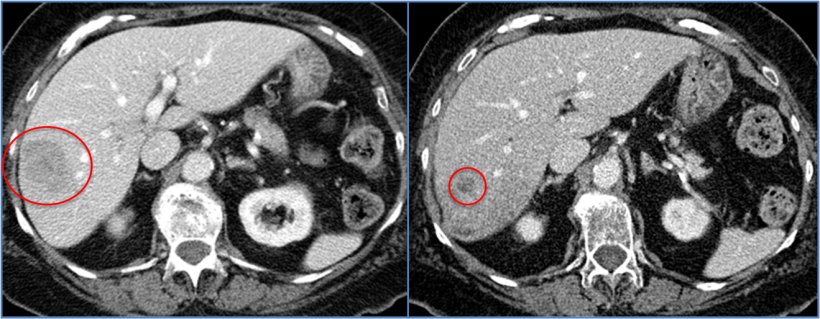
Image source: Dr Lewandowski
Finding the right patient groups
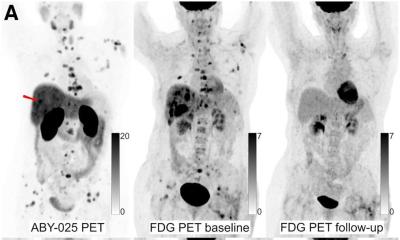
Another study conducted on 81 patients injected with resin microspheres reported on the safety, efficacy, and prognostic factors after radioembolization of hepatic metastases from breast cancer.3 ‘Results showed a 30% decrease in maximum standardized uptake value on FDG-PET for up to five treated lesions in 52% of patients,’ he said. ‘Radioembolization had the biggest impact in patients with baseline normal liver function and limited liver disease burden.
Emerging data on local intra-arterial therapy for metastatic breast cancer demonstrates that radioembolization is safe, preserves quality of life and stops disease progression
Robert Lewandowski
Most recently, several studies have evaluated factors to consider when selecting best patients for radioembolization. These include estrogen-receptor positive patients, bone-only extra-hepatic metastases, and radioembolization performed earlier in the disease course (within six months after initial breast cancer metastases diagnosis).4 ‘Emerging data on local intra-arterial therapy for metastatic breast cancer demonstrates that radioembolization is safe, preserves quality of life and stops disease progression,’ Lewandowski said. ‘It also allows reinitiating of chemotherapy in 67% of the patients if that option remains.’ A few small cases series have shown the potential benefit of combining local and systemic therapy in this patient population.
An interesting concept is combining immune therapy with radioembolization. Recent work published in the Journal of Vascular and Interventional Radiology has studied genetic profiling, finding a potential benefit of combining radioembolization with immune checkpoint inhibitors to improve outcomes.5
Future evaluation will have to focus on optimizing patient selection and considering that application of radioembolization earlier in the course of disease, Lewandowski suggested. ‘We should further assess the efficacy of radioembolization in combination with systemic therapies,’ he concluded.
References:
- Feretis M, Solodkyy A: Yttrium-90 radioembolization for unresectable hepatic metastases of breast cancer: A systematic review; World Journal of Gastrointestinal Oncology 2020
- Gordon et al.: Yttrium-90 radioembolization stops progression of targeted breast cancer liver metastases after failed chemotherapy; Journal of Vascular and Interventional Radiology 2014
- Fendler et al.: Safety, Efficacy, and Prognostic Factors After Radioembolization of Hepatic Metastases from Breast Cancer: A Large Single-Center Experience in 81 Patients; Journal of Nuclear Medicine 2016
- Barakat et al.: Transarterial Yttrium-90 Glass Microsphere Radioembolization of Chemotherapy-Refractory Breast Cancer Liver Metastases: Results of a Single Institution Retrospective Study; Advances in Radiation Oncology 2022
- Zhan et al.: Safety of Combined Yttrium-90 Radioembolization and Immune Checkpoint Inhibitor Immunotherapy for Hepatocellular Carcinoma; Journal of Vascular and Interventional Radiology 2020
06.02.2023