Source: University of Manchester
News • Acute myeloid leukaemia
AML's Achilles’ heel opens door for new treatments
New findings about a fatal form of blood cancer could aid the development of new drugs with significantly less harmful side effects than existing chemotherapy.
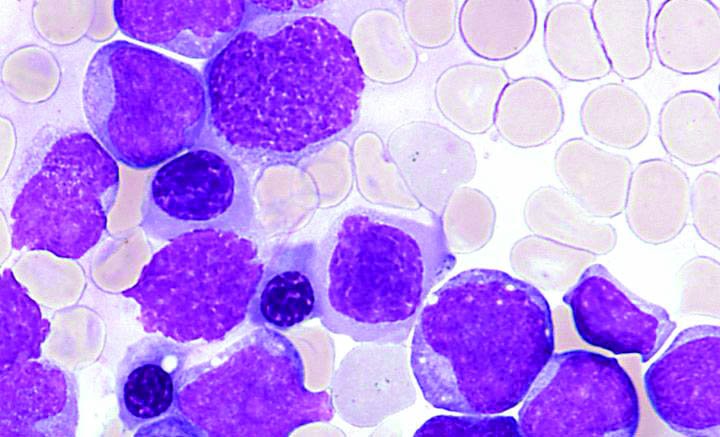
The discovery could lead to novel treatments that efficiently eliminate blood cancer cells in acute myeloid leukaemia (AML), without harming healthy blood cells. Researchers have discovered how a protein in the body plays a key role in AML – an aggressive cancer of white blood cells with very poor survival rates. The study showed that the protein, known as YTHDF2, is needed to trigger and sustain the disease, but is not needed for healthy cells to function. This identifies YTHDF2 as a promising drug target for leukaemia.
A team of researchers led by the University of Edinburgh and Queen Mary University of London carried out a series of experiments to understand the role of YTHDF2 in blood cancer. The study, carried out in collaboration with The University of Manchester, Harvard Medical School and the Université de Tours, was published in Cell Stem Cell. It was supported by Cancer Research UK and Wellcome.
Recommended article

News • Acute myeloid leukaemia
Researchers draw AML ‘family trees’ in patients treated with enasidenib
For the first time, a team of international researchers have mapped the family trees of cancer cells in acute myeloid leukaemia (AML) to understand how this blood cancer responds to a new drug, enasidenib. The work also explains what happens when a patient stops responding to the treatment, providing important clues about how to combine enasidenib with other anti-cancer drugs to produce…
Our work sets the stage for therapeutic targeting of cancer stem cells in leukaemia while enhancing the regenerative capacity of normal blood stem cells
Kamil Kranc
Tests in blood samples donated by leukaemia patients showed that the protein is abundant in cancer cells, while experiments in mice found that the protein is required to initiate and maintain the disease. Further tests enabled scientists to determine the biological pathway by which interfering with the function of YTHDF2 selectively kills blood cancer cells. Importantly, they also showed that the protein is not needed to support the function of healthy blood stem cells, which are responsible for the production of all normal blood cells. In fact, blood stem cells were even more active in the absence of YTHDF2.
Professor Dónal O’Carroll, of the University of Edinburgh’s School of Biological Sciences, who co-led the research, said: “The study shows the promise of a novel class of drugs as the basis for cancer and regenerative medicine treatments.” Professor Kamil Kranc, of Barts Cancer Institute, Queen Mary University of London, who jointly led the study, said: “Our work sets the stage for therapeutic targeting of cancer stem cells in leukaemia while enhancing the regenerative capacity of normal blood stem cells. We hope this will establish a new paradigm in cancer treatment”.
Source: University of Edinburgh
26.04.2019