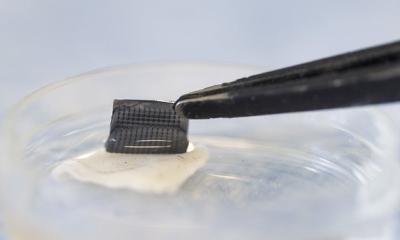
Image source: Mirbeik et al., Scientific Reports 2022 (CC BY 4.0)
News • Dermatology tool
Skin cancer detection: handheld device as painless alternative to biopsy
Skin biopsies are rather unpleasant, but remain an important tool for early detection of cancer. However, in recent years, aggressive diagnostic efforts have seen the number of biopsies grow around four times faster than the number of cancers detected, with about 30 benign lesions now biopsied for every case of skin cancer that’s found.
Researchers at Stevens Institute of Technology are now developing a low-cost handheld device that could cut the rate of unnecessary biopsies in half and give dermatologists and other frontline physicians easy access to laboratory-grade cancer diagnostics. “We aren’t trying to get rid of biopsies,” said Negar Tavassolian, director of the Bio-Electromagnetics Laboratory at Stevens. “But we do want to give doctors additional tools and help them to make better decisions.”
The researchers published their findings in the journal Scientific Reports.
There are other advanced imaging technologies that can detect skin cancers, but they’re big, expensive machines that aren’t available in the clinic
Negar Tavassolian
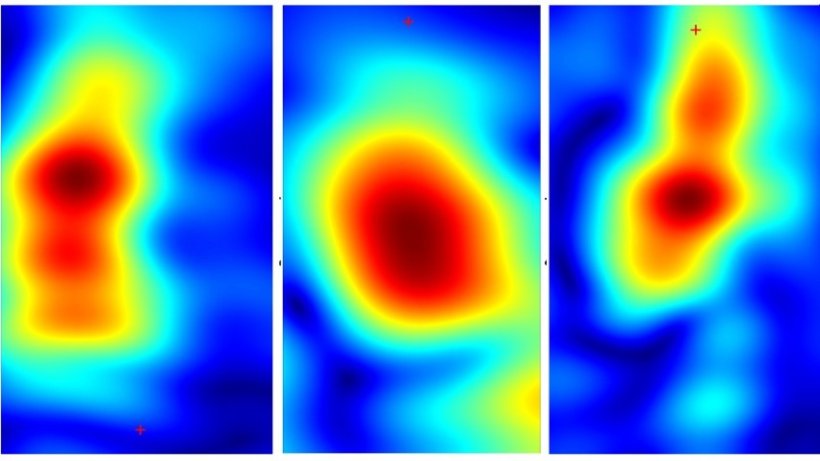
The team’s device uses millimeter-wave imaging — the same technology used in airport security scanners — to scan a patient’s skin (In earlier work, Tavassolian and her team had to work with already biopsied skin for the device to detect if it was cancerous). Healthy tissue reflects millimeter-wave rays differently than cancerous tissue, so it’s theoretically possible to spot cancers by monitoring contrasts in the rays reflected back from the skin. To bring that approach into clinical practice, the researchers used algorithms to fuse signals captured by multiple different antennas into a single ultrahigh-bandwidth image, reducing noise and quickly capturing high-resolution images of even the tiniest mole or blemish.
Spearheaded by Amir Mirbeik Ph.D. ’18, the team used a tabletop version of their technology to examine 71 patients during real-world clinical visits, and found their methods could accurately distinguish benign and malignant lesions in just a few seconds. Using their device, Tavassolian and Mirbeik could identify cancerous tissue with 97% sensitivity and 98% specificity — a rate competitive with even the best hospital-grade diagnostic tools. “There are other advanced imaging technologies that can detect skin cancers, but they’re big, expensive machines that aren’t available in the clinic,” said Tavassolian. “We’re creating a low-cost device that’s as small and as easy to use as a cellphone, so we can bring advanced diagnostics within reach for everyone.”
Because the team’s technology delivers results in seconds, it could one day be used instead of a magnifying dermatoscope in routine checkups, giving extremely accurate results almost instantly. “That means doctors can integrate accurate diagnostics into routine checkups, and ultimately treat more patients,” said Tavassolian. Unlike many other imaging methods, millimeter-wave rays harmlessly penetrate about 2mm into human skin, so the team’s imaging technology provides a clear 3D map of scanned lesions. Future improvements to the algorithm powering the device could significantly improve mapping of lesion margins, enabling more precise and less invasive biopsying for malignant lesions.
The next step is to pack the team’s diagnostic kit onto an integrated circuit, a step that could soon allow functional handheld millimeter-wave diagnostic devices to be produced for as little as $100 a piece — a fraction of the cost of existing hospital-grade diagnostic equipment. The team is already working to commercialize their technology and hopes to start putting their devices in clinicians’ hands within the next two years. “The path forward is clear, and we know what we need to do,” said Tavassolian. “After this proof of concept, we need to miniaturize our technology, bring the price down, and bring it to the market.”
Source: Stevens Institute of Technology
05.05.2022