Article • Today’s improved lower leg treatments
Peripheral vascular therapies
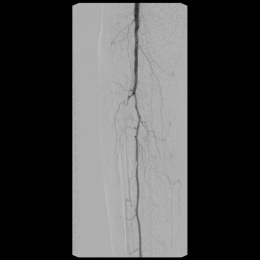
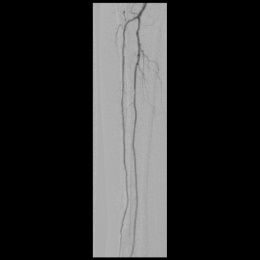
Interventional radiotherapy for tibial arteries has increased in recent years. Why? People are getting older and better techniques and materials now permit treatment even of very thin vessels. Professor Dierk Vorwerk, Director of the Institute for Radiology at Ingolstadt Hospital, where almost a third of all interventions in his department are performed on the lower leg, described the most important innovations.
Interview: Daniela Zimmermann

Blood vessels in the lower leg form a fine structure in the upper range of three millimetres and lower range no more than 1.5mm. With the wires and balloon catheters available in the past only limited interventions were possible. Meanwhile the wires and instruments are more delicate and above all more versatile. Thus, in addition to balloon catheters that are up to 20 cm long today, there are so-called support catheters. They are tapered at the tip, very stable, and support the process of pushing by expanding the vessel in front. The stability can also be improved by use of additional guide catheters or sluices.
New on the market are also atherectomy systems that work like a milling machine, removing the plaque from the walls of the vessels and pulverising it. With new materials come new methods. If access cannot be obtained through the groin, then the vessel is punctured exactly behind the stenosis in the tibia and then opened from there in reverse. That also functions through the foot arch.
‘We call this rendezvous technique when the access is sought equally from above and below,’ Vorwerk explained. However, these special techniques are more of an exception in his department. ‘The work from the ipsilateral groin usually works well, so I can dispense with special techniques.’ Installing catheters in a crossover procedure is another matter. In this case work begins from the opposite side, a disadvantage since, due to the longer distance and loss of energy in the aortal bifurcation, it is not possible to use full force. Access from below can be chosen as an alternative.
Where is the intervention?
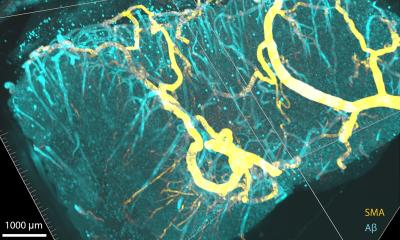
Along with the anterior and posterior arteries, there is the arteria fibularis deep in the middle. For most patients this is the most important vessel, since its strong collateral supplies blood to the foot—even when nothing else helps any more. In addition, the vessels below the ankle are dilated and not even with very bad results, although the data situation is rather thin. The knee artery is the main line for blood supply to the lower leg. It often exhibits heavy calcification, leading to restrictions in the foot.
However, a stent implantation at the level of the joint line is disadvantageous. The collaterals from the deep femoral arteries that end above and below the knee are important for supplying the leg and can partially compensate for constrictions in the knee artery.
The time for treatment?
The peripheral vascular illnesses are described according to the Fontaine or Rutherford classification. The serious stages lead to static pains (Fontaine III, Rutherford 4) or trophic disorders; often accompanied by open wounds, black toes and similar symptoms (Fontaine IV, Rutherford 5-6). ‘We treat the lower leg arteries starting with stage III, that is with the incidence of static pain or trophic disorders.’ The only exception: if patients have an isolated narrow stenosis of truncus tibiofibularis causing calf pains when walking then Vorwerk intervenes earlier.
The main objective: wound healing
A decisive criterion for an intervention’s clinical success is the functioning of the small arterioles. There are patients for whom the vessel can be opened very well but without any improvement in the blood supply to the tissue. The reason is that the small vessels are no longer able to transport the increased blood volume to the tissue that is sent to the foot. Frequently this cannot be judged in advance. There is current work being done on tests for more certain prognoses.
Interventions in the tibial arteries are not intended primarily to keep the vessel open for the long-term. Rather, precedence is given to healing the wound on the foot and returning the patient to a stable stage 2b. ‘Wound healing, and thus conservation of the foot and lower leg tissue, that is to say avoiding amputation, is the main issue – naturally with the diabetic foot, but not only there. Compared to that, elimination of patient pain while walking is rather secondary.’ After all, most of these patients no longer walk very much and, as diabetics, also no longer have any pronounced sensitivity to pain.
Percutaneous balloon catheterisation before bypass and stents
The last resort with a blocked vessel is also the very controversial sympathicolysis. Here the sympathetic nerve network in the back is destroyed to force a widening of the vessels
Dierk Vorwerk
In the context of the vascular conference, angiologists, cardiologists, nephrologists and radiologists clarify the responsibilities and discuss the planned intervention. ‘Usually we prefer a percutaneous balloon first. If that does not work, then a bypass is set. We have become more cautious here however since once set a new opening is often difficult. In addition, the consistency results are not optimal. The last resort with a blocked vessel is also the very controversial sympathicolysis. Here the sympathetic nerve network in the back is destroyed to force a widening of the vessels.
Stents do not play much of a role in the lower leg: the lesions are sometimes more than 20 cm long and stents of this size are rare.
No reimbursement for drug-eluting balloons
The use of drug-eluting balloons is currently in dispute. The initial findings of a large-scale study have been really convincing. The procedure also suffers from the fact that a health insurer does not absorb the costs. Additionally, a meta-analysis has shown that the mortality rate for patients treated with coated balloons was higher than those without drugs: ‘Although the difference was very small, it was still significant.’
These uncertainties have meant that drug-eluting balloons are only used if the patient explicitly consents after thorough explanation.
Possible candidates for a repeat intervention with a drug-eluting balloon, despite the risk are patients exhibiting a new constriction after only three months, or who have developed a pronounced neointimal hyperplasia in a stent.
Profile:
Professor Dierk Vorwerk, co-founder (in 2008) of the German Society for Interventional Radiology and Minimal Invasive Therapy (DeGIR) has directed the Institute for Diagnostic and Interventional Radiology at the Klinikum Ingolstadt for 21 years. He is a renowned author of numerous scientific papers and book contributions and is a member and honorary member of many national and international specialty societies. He has also chaired the DeGIR (2012-2014) and was President of the German Röntgen Society (2015-2017).
31.10.2019