Image source: Adobe Stock/Deemerwha studio
Article • UK research project
"Our Future Health": Shifting from curative to preventive care
In the face of increasing longevity and the rise of chronic diseases in later life, shifting from curative to preventive care will become vital for healthcare systems as they primarily focus on treating symptomatic individuals in the late stages of diseases.
Report: Cornelia Wels-Maug
The UK’s National Institute for Health and Care Research, for example, predicts that by 2035, 67.8% of those aged 65 will have at least two serious conditions or impairments, up from 54% in 2015. Sir John Bell, Regius Professor of Medicine at Oxford University, concludes that as the burden of chronic diseases is escalating, health systems must address underlying pathologies rather than focus primarily on managing late-stage diseases: 'Before you know it, the health system is overwhelmed by late-stage disease that is very, very difficult to manage,' the expert finds.
Right now, we treat people at high costs three months before they die
Sir John Bell
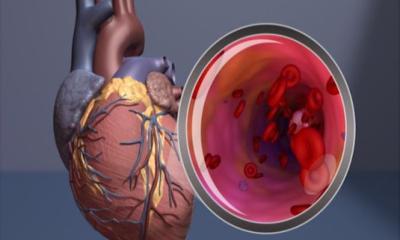
The key challenge lies in addressing the underlying pathologies before they manifest as symptoms. Bell emphasizes the need to transition healthcare from a broad, reactive approach to a targeted, preventive one. This shift, he argues, not only enhances individuals' quality of life but also alleviates financial strains on healthcare systems. At the Economist Impact event "Future of Health 2023 Europe" in October 2023, Bell proposed a prevention agenda that identifies high-risk individuals and intervenes with behavioural changes that delay either the onset of a disease or make it obsolete: 'Right now, we treat people at high costs three months before they die. However, identifying and treating chronic diseases before they show symptoms, increases the efficacy of therapies,' explains Bell.

Image source: University of Oxford
He proposes a targeted approach, concentrating resources on populations at risk rather than adopting a broad strategy. 'What you need to do is concentrate your resources on the people who are going to suffer from a disease rather than the whole population,' he says. 'Up until recently, we haven’t really been able to do that, because we have had to do everything to everybody, which is massively inefficient. However, developments in the last five to ten years such as large-scale epidemiology as well as molecular tools such as biomarkers and genome sequencing have paved the way for a more preventative approach to healthcare.'
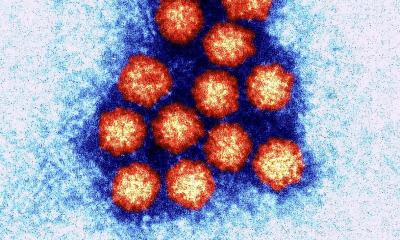
Based on the results of genome sequencing, polygenic risk scores can establish a measure of an individual’s risk to develop a specific medical condition due to one’s genes. Combining polygenic risk scores with other factors that influence disease risk allows for a more accurate estimation of how likely a person is to develop a specific disease than considering either alone. The algorithms used for calculating those likelihoods are based on artificial intelligence (AI). All of these approaches complement traditional measures like blood pressure and cholesterol levels and offer a gamut of tools for a prevention-centered healthcare delivery.
Paradigm shift: Putting preventative healthcare into action
The UK’s Our Future Health programme, which Bell chairs, exemplifies the paradigm shift to a prevention-centered healthcare approach. The goal is to revolutionize healthcare by combining genetic analysis with lifestyle data, providing insights into human health on an unprecedented scale. The study aims to explore the potential uses of genetic risk scores in health screening, facilitating the development of new ways to identify diseases before they become symptomatic as well as to improve health outcomes and life quality.
The project targets to recruit five million volunteers by 2025 and collect comprehensive data on their genetics, health, and lifestyle to understand the factors influencing health conditions. The initial focus of the study lies on cancer, Alzheimer’s, heart disease, arthritis, diabetes and stroke. Our Future Health, which is the UK’s largest ever health research programme, also wishes to showcase that collecting these data inexpensively can significantly impact health outcomes. 'Now you can tell people at the age of 25 that they are in the top 5% of risk for cardiovascular disease, so they need to pay attention to it,' says Bell.
We set out to create a health research programme on a scale never seen before anywhere in the world. Hitting one million volunteers over the last year is a truly remarkable achievement and means we’re now rapidly turning that ambition into reality
Sir John Bell
Although invitations to sign up for the programme were sent out initially to households in West Yorkshire, West Midlands, Greater Manchester and Greater London, any resident in the UK above 18 can partake. The first volunteer signed up on July 12th, 2022, and by January 19th, 2024, the number of participants had grown to 1,163,710 with about 3,000 new people joining daily. Volunteers’ data will be de-identified and held in "trusted research environments" that meet strict security criteria. An access board, including independent experts and members of the public, will ensure the resources are only used for health research in the public interest. 'When we started Our Future Health, we set out to create a health research programme on a scale never seen before anywhere in the world. Hitting one million volunteers over the last year is a truly remarkable achievement and means we’re now rapidly turning that ambition into reality,' Bell concludes.
Our Future Health is run by a charity of the same name and is supported by the UK government together with the NHS. It is set up as a public private partnership with partners from the industry as well as disease-related charities, both groups bringing their expertise in discovering and developing new prevention and treatment methods to the table. A third of its £239 million budget is financed from UK Research and Innovation with the remaining funds coming from leading life sciences companies and charities. Although initial recruitment of volunteers is planned to be concluded by end-2025, they will remain enrolled for life unless they decide otherwise, making for a long outlook of the programme.
25.01.2024