© Asim Sheikh
Article • Precision approach through the eye socket
Orbital gateway to surgical removal of brain tumours
Using a keyhole surgery approach, surgeons have found a new way to access previously difficult-to-reach brain regions with faster recovery times. With the help of 3D modelling technology, the neurosurgeons succeeded in removing complex tumours from the cavernous sinus through the eye socket, avoiding complex brain surgery and enabling their patients to make a quicker recovery.
By Mark Nicholls

© Leeds Teaching Hospitals NHS Trust
‘The primary advantage is that it provides direct access to the cavernous sinus, which was once thought to be an inaccessible area,’ explains Consultant Neurosurgeon Asim Sheikh from Leeds Teaching Hospitals Trust in the UK, one of the European centres performing this procedure. ‘This allows safer removal of tumours without the risk of injuring or retracting brain tissue, which would otherwise be required with traditional craniotomy.’
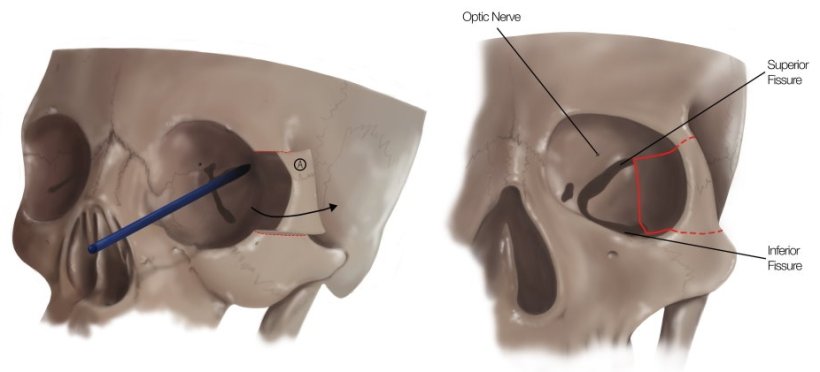
The procedure begins with a small 1-1.5 cm incision at the outer edge of the eye, followed by an internal incision within the eye lining to access the bones. Surgeons then carefully cut a small segment of bone in the outer wall of the eye socket, keeping it attached to tissues and muscles while pushing it outward to create space for surgical instruments. The final step involves drilling the back wall of the eye socket to gain access to the tumour.
This minimally invasive approach leaves patients with only a tiny scar near the eye, reducing recovery time. The first UK patient – a 40-year-old stroke nurse with a meningioma in the cavernous sinus – returned to work within just three months of her surgery.
3D technology for optimal preparation
Given the procedure's complexity, surgeons at Leeds utilized advanced 3D modelling technology to rehearse the operation before entering the OR, building a 1:1 scale model to plan the surgery. Mr. Sheikh, who works alongside Consultant Maxillofacial Surgeon Jiten Parmer, added that preparation involves neuro-navigation software with 3D segmentation of all structures to virtually perform the surgery, complemented by practice sessions in the cadaver lab.
Lisa Ferrie, the Trust's Biomedical Engineer and 3D Planning Service Lead, notes that the 3D technology enables the surgical team to study patient anatomy and prepare for the procedure ‘with unparalleled accuracy,’ significantly enhancing surgical precision.
Recommended article

Article • Technology applications
Medical 3D printing: from niche to mainstream
From personalized medical guides and implants to advanced surgical planning solutions: 3D printing and visualization has seen considerable growth over the past years and is already making a significant impact in healthcare. AI, cloud, and virtual/augmented reality technologies show promise to further advance the number of applications.
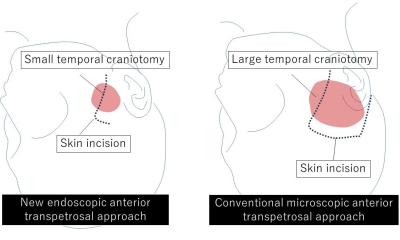
Previously, an operation to remove such a tumour would require complex brain surgery involving craniotomy and taking a large part of the skull away – risking complications that could include brain injury and seizures, Sheikh said. ‘It’s a hard-to-reach area,’ he continued, ‘but this new approach allows direct access without any compromise of pressure on the brain. We can now reach areas which were once thought to be inoperable, but now are accessible.’
Initially established for trauma patients, the technique was adapted for brain tumour surgery by teams in South Korea and Barcelona, Spain – where Mr. Sheikh trained before introducing it to Leeds in 2023. Neurosurgeons in New York further developed the approach, which is now being taught to specialists in Oxford, Bristol, Edinburgh, and Liverpool. The Leeds team has successfully performed six such operations for tumours. Mr. Sheikh explained that this approach offers the ability to remove tumours that were previously thought difficult to remove, or even inoperable.
Substantial benefits for patients
Depending on tumour size and consistency, the procedure takes 4-10 hours under general anaesthesia. While there is a risk to affect the patient’s eyesight, Mr. Sheikh explains their technique minimizes this concern: ‘In our technique, we create room by removing a portion of the outer wall of eye socket and that minimises this risk. We have not had any visual complications so far.’
The benefits to patients have been reported to be substantial: quicker recovery, early mobilization, faster discharge home, reduced risk of brain injury, and superior access to deep-seated tumours. As this technique continues to develop, it represents a significant advancement in the treatment of complex brain tumours, offering hope to patients who previously had limited options, the team summarizes.
Profile:
Mr Asim Sheikh is Consultant Neurosurgeon with subspecialist expertise in skull base and neurovascular surgery at the Leeds General Infirmary. His specialist interests include endoscopic endonasal skull base surgery, open skull base neurosurgery, minimal access surgery and brain tumour surgery. He is a member of the Royal College of Surgeons of England, the Society of British Neurological Surgeons and the British Neurovascular group.
09.06.2025