Handheld
Multiphoton microscope and endoscope could speed up diagnosis
Two new optical devices could reduce the need to take tissue samples during medical examinations and operations and to then send them for testing – potentially speeding up diagnosis and treatment and cutting healthcare costs.

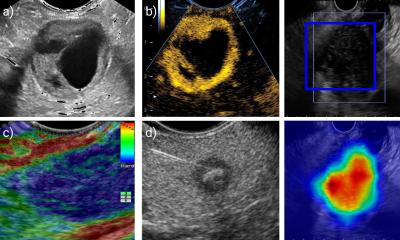
One is a lightweight handheld microscope designed to examine external tissue or tissue exposed during surgery. One example of its use could be to help surgeons compare normal and cancerous cells (during an operation). A key advantage is that the device can acquire high quality 3D images of parts of the body while patients are moving (eg due to normal breathing), enabling it to be applied to almost any exposed area of a patient’s body.
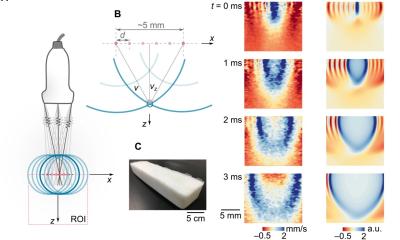
The second instrument, a tiny endoscope incorporating specially designed optical fibres and ultraprecise control of the light coupled into it, has the potential to be inserted into the body to carry out internal cell-scale examination, for example during neurosurgery. Ultimately, this new approach may be able to provide high resolution images enabling surgeons to see inside individual cells at an adjustable depth beneath the surface of the tissue.
Both prototypes have been developed by Imperial College London in collaboration with the University of Bath and funded by the Engineering and Physical Sciences Research Council (EPSRC).
Currently, the diagnosis of many diseases requires taking a tissue specimen from the patient, preparing it in a laboratory, studying it under a microscope and then forwarding the results back to the clinician. The new devices, both of which harness a technique known as multiphoton excited fluorescence microscopy* to analyse individual cells in their native tissue, could be used in a consulting room or an operating theatre to help clinicians identify diseased tissue and provide a rapid diagnosis.
The handheld microscope incorporates a tracking mechanism that compensates for the patient’s movements, ensuring the generation of steady images. The endoscope is just a fraction of a millimetre in diameter and has no moving parts. Both these devices use novel multicore optical fibres developed by Imperial’s collaborators by the University of Bath.
Dr Chris Dunsby of Imperial College London, who has led the overall project, says: “These new devices open up exciting possibilities in the field of in-situ diagnosis and could help improve patient care in the future.”
Professor Jonathan Knight, who led the University of Bath team, says: “This has been a very exciting project which has enabled us to develop fibres with performance which we would have previously thought impossible.”
After further development and refinement of the technology, clinical trials will explore the healthcare benefits of the two devices in more detail, with the goal of beginning to introduce them into clinical use within around 5-10 years.
* This technique involves illuminating tissue with light of a specific wavelength that causes molecules in the tissue to emit light in response. This emission is called autofluorescence and can be used to form high-resolution images that could help determine whether, and to what extent, the tissue is diseased. Multiphoton excitation is where the required excitation is provided by two photons of half the required energy that are absorbed simultaneously. For tissue autofluorescence, this means that the illuminating photons can be near infrared rather than visible light and therefore can penetrate deeper into biological tissue – enabling 3D images to be produced up to ~0.1mm beneath the tissue surface in clinical instruments.
Source: Engineering and Physical Sciences Research Council (EPSRC)
27.05.2016