Genomics
MRI holds predictive potential in oncology
The ‘MRI of the Adnexa, Essentials and Beyond’ session from at the MR 2015 symposium held in Garmisch, Austria, presented tips and tricks in clinical routine before moving to research that combines imaging and genomic data to better evaluate ovarian cancer.
Report: John Brosky

‘It is very important to be able to say a lesion is benign and is not a cancer,’ said Evis Sala MD PhD, Director of Body Imaging Services at the Memorial Sloan-Kettering Cancer Center in New York City. ‘It may be easier to say that you cannot exclude malignancy, but this is completely unhelpful to the referring physician, and especially the patient.’ Such inconclusive diagnoses, she added, leave the medical team with few options.
In the first part of her presentation during the MR 2015 Garmisch symposium, Dr Sala focused on what she calls the essentials of magnetic resonance imaging of the adnexa region, and also included tips and tricks to achieve a highly accurate characterisation of ovarian lesions and how to avoid the pitfalls of mimickers of malignancy.
‘It is absolutely possible, especially with MRI, to make a specific diagnosis of whether a lesion is benign or malignant in about 90% of cases – and this is what’s essential, to make a difference right now for the patient on the table,’ she emphasised. ‘It is not only our goal but the reason for our existence as clinical radiologists.’
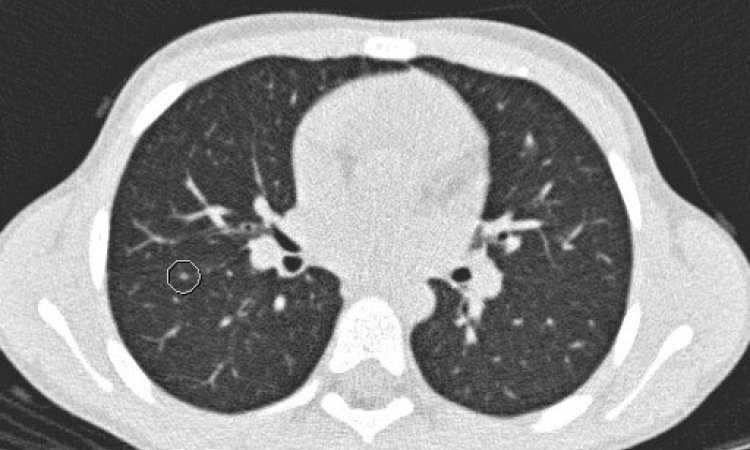
In a second stage, Dr Sala described evolutions in multiple MR sequences that have been in use in clinical routine for several years but which, she pointed out, keep getting better. ‘We know that MRI can show anatomy better, but it also has the added value, with additional sequences, to show physiology as well, which is often called functional imaging. With diffusion-weighted imaging we can interrogate cellular density and the integrity of the cellular membrane. With perfusion imaging we can probe vascularity within the lesion, both key in evaluating malignant lesions as well as assessing treatment response in cancer and even for predicting response,’ she said.
In this segment of the presentation Dr Sala highlighted advanced techniques and methods for MRI currently being used in clinical trials and for research to predict treatment outcomes.
She said she wanted to avoid the tendency to focus only on imaging. ‘Radiologists should not practice in isolation. We need to integrate clinical information with imaging to provide an accurate diagnosis. I like to know the patient’s age and all her symptoms, and all the lab reports before I look at the images. I put a lot of emphasis on this.’
Integration of multiple disciplines proved to be the major theme for the final part of Dr Sala's talk, which moved to next-generation imaging that combines MRI capabilities with pathology and genomics. ‘I say we are moving beyond current MRI because we can actually step forward to understand the heterogeneous biology of ovarian cancer, to link imaging phenotypes with genotypes in order to identify the metastatic potential.
‘This is very early work from my current research that I want to share with the audience as a kind of future for MRI,’ she added. ‘This research is focused on establishing the benchmarks, to establish a proof of principle. Once we can say that there is an underlying genomic basis for an imaging phenotype then, in the future perhaps, we will be able to use imaging to guide treatment decisions and avoid multiple biopsies,’ she predicted. ‘We can’t biopsy 10 times, so that a patient becomes a pincushion. There is a limit. What we are doing is validating MR imaging as a virtual biopsy tool.
‘Moving beyond MRI means that today we know what is cancer and what is not,’ she said. ‘Now we are asking how can we delve further and have a greater insight into the biology of the heterogeneity, the underlying genomic composition of the cancer? We are asking if we can identify the clones that have metastatic potential and the ones that can drive a resistance to therapy.’
Recent technological advances have brought complementary innovations in genomics that, when coupled with innovations in MRI imaging, allow the spatial quantification of tumour heterogeneity and the clonal composition of the genomics, as well as how they change during treatment. ‘Hopefully this will provide, in the future, the basis for improved treatment and outcomes,’ she said. ‘We want to have personalised cancer therapies, and this may be a fundamental driver for this personalised oncology.’
More than getting the right drug to the right patient at the right moment, Dr Sala said effective cancer therapy could also be a question of getting the drug to the right part of a tumour. ‘We know that tumours are different, that they are composed of different habitats, different clusters. Some of these clusters will drive the resistance to chemotherapy – and this is what actually kills the patient,’ she pointed out. ‘If we can know, by evaluating the different parts of the tumour, which one will drive resistance to the standard chemotherapy, we may be able to offer a new drug immediately to a patient.’
Moving forward also means that radiology needs to move beyond recognising patterns with the naked eye. Interpreting a visual image is the basis of radiology and it remains valid in everyday clinical practice and will never go away, Dr Sala underlined. Yet today there is much more that an MR image can offer through quantifiable data that can be extracted. Integration of diverse and complex data requires a team, she said. At Memorial Sloan-Kettering the team consists of physicists, bio-informaticians, a geneticist, pathologists, oncologists, surgeons and radiologist. ‘This is how we need to work now,’ she said. ‘We already work on disease management teams where multiple specialists come together. The time when the radiologist works alone is gone.’
PROFILE:
Evis Sala is the Chief of the Body Imaging Service and Director of Gynaecologic Imaging at the Memorial Sloan Kettering Cancer Center. Her current translational research aims to transfer new multimodality functional imaging techniques from the laboratory to clinical use. Before joining the MSKCC staff in 2012, Dr Sala was a University Lecturer in Radiology and Specialty Teaching Director (Radiology) at the University of Cambridge, United Kingdom, as well as an Honorary Consultant Radiologist at Addenbrooke’s Hospital, Cambridge, where she served for seven years as the Lead Clinician for Gynaecology Imaging. A medical graduate from University of Tirana, Albania (1991), Dr Sala gained her PhD at the University of Cambridge (2000), where she also completed her Clinical Radiology training (2005).
07.03.2015