
Image source: Adobe Stock/New Africa
News • Q&A on research, diagnosis, treatment
Endometriosis: More than just ‘painful periods’
A Yale Medicine expert explains the latest thinking on this difficult-to-diagnose disease.
Even though endometriosis affects an estimated 10% of reproductive-age women in the United States and can cause increasing, debilitating pain each menstrual cycle, as well as infertility, it is often misdiagnosed and misunderstood. Part of the problem is that endometriosis is not a straightforward disease; researchers are learning how it can involve multiple organs and occur across the entire body. The disease gets its name from the endometrium, the lining of a woman’s uterus. In endometriosis, endometrial tissue grows outside the uterus—on the bowels and/or ovaries, as well as behind the uterus and elsewhere.
During a normal menstrual cycle, the endometrium thickens and is shed. With endometriosis, though, the tissue outside the uterus is shed into the abdomen. The shedding that occurs each month with menstruation causes pain, inflammation, and scar tissue, which is why the condition is often associated with painful periods. “The degree of pain can be far worse than what any woman should expect with her monthly period, especially since it is a progressive disease, meaning that scar tissue accumulates and the pain worsens over time,” says Hugh Taylor, MD, chair of Yale Medicine Obstetrics, Gynecology & Reproductive Sciences. A leading endometriosis researcher, Dr. Taylor hopes that recent discoveries around the disease will make it easier to diagnose and treat.
Statistics show that women will see four or five practitioners before they get the right diagnosis and that more than half are misdiagnosed initially
Hugh Taylor
“Endometriosis is a disease that is still under-recognized and under-treated—both by women suffering from it and health care providers,” Dr. Taylor says. “The first symptom of the condition often is painful periods. With pain in any other region of the body, doctors immediately investigate to find out what’s wrong; however, this is the only pain that the medical community considers ‘normal.’ Pain with menses is far too frequently dismissed. That attitude can leave patients questioning whether their pain is truly different—or worse—than someone else’s.”
Furthermore, many women, especially those who are younger, are reluctant to discuss other symptoms that can accompany endometriosis, such as pain with bowel movements or during intercourse, he adds. “Statistics show that women will see four or five practitioners before they get the right diagnosis and that more than half are misdiagnosed initially,” Dr. Taylor says.
Below, we talked more with Dr. Taylor about endometriosis and ongoing research that holds promise for better understanding and treatment of the disease.
Q: How does endometriosis affect the entire body?
Over the past decade, research has shown that endometriosis may be a chronic, systemic disease that affects the entire body and not just a single organ or body part.
“Our research has shown that the inflammation from endometriosis can activate white blood cells and create inflammation throughout the body,” says Dr. Taylor, adding that microRNA molecules (which help control gene expression) differ in women with endometriosis. “They can travel to different organs. They have a hormone-like effect, and we have shown that microRNAs are a major signaling mechanism that creates these whole-body effects.”
Recommended article
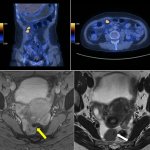
Article • Ovarian cancer and endometriosis detection
Women’s health imaging: PET/CT and T2*w MR show promise
Diagnostic imaging in women’s health advances: PET/CT might provide a more accurate imaging alternative to CT in ovarian cancer. T2*-weighted MR imaging in deep endometriosis detection also shows promise, but ultimately falls flat.
Q: What are some new research findings about endometriosis?
Our understanding of the disease is changing, Dr. Taylor says. One example relates to the fact that women with endometriosis tend to be thinner. “Many medical textbooks say, ‘Being underweight is a risk factor for endometriosis.’ And women would sometimes be told, ‘You're not eating enough,’ as though the condition is their fault,” he says. “But our research, using animal models, has suggested that having low body fat and being thin may be caused by endometriosis. Changes in the mice’s fat cells in our studies explain the weight loss; their metabolism has been changed.”
I’ve heard disparaging things said about patients, such as, ‘You’re anxious and complaining a lot—just relax and don’t worry about the cramps.’ That attitude is demeaning
Hugh Taylor
Another example, Dr. Taylor adds, is that epidemiologic studies have shown that as women with endometriosis age, they have a higher incidence of cardiovascular disease, which was previously attributed to the medications used to treat endometriosis. Another risk factor for cardiovascular disease, he says, is hysterectomy (the surgical removal of the uterus), which can be used to treat endometriosis. “But, again, studies now show that endometriosis itself, without hormonal treatments or hysterectomy, increases rates of atherosclerosis [the buildup of cholesterol plaque in the artery walls],” Dr. Taylor says. “Research also shows that women with endometriosis have higher rates of depression and anxiety. I’ve heard disparaging things said about patients, such as, ‘You’re anxious and complaining a lot—just relax and don’t worry about the cramps.’ That attitude is demeaning.”
In Dr. Taylor’s studies, he and his team created endometriosis in mice. “Endometriosis led to differences we observed in gene expression and nerve conduction in the brain. A few weeks after we induced the endometriosis, the mice became more depressed, more anxious, and more sensitive to the painful stimuli than they were prior to the induction,” he says. This, Dr. Taylor adds, is something also seen in women with endometriosis. “They have what’s called ‘central sensitization of pain,’ in which those with the condition are more sensitive to the same painful stimuli than they were before having endometriosis,” he says.
Q: Why does it take so long to diagnose endometriosis?
Not understanding the systemic effects explains why an endometriosis diagnosis, on average, takes 10 years, Dr. Taylor explains.
Endometriosis causes a vast number of symptoms in multiple organs that can mimic other disease processes. “So, instead of focusing on one disease, doctors will refer women to up to five different subspecialists. ‘You have an intestinal problem, see a gastroenterologist; you have a psychiatric problem, see a psychiatrist; you're underweight, see a nutritionist,’ and so on. That causes a tremendous delay in diagnoses,” he says.
Recommended article

Article • Women's health
Benign gynaecology specialist centres are needed
The recently opened Uterine Repair Center (URC) in VUmc (Amsterdam) serves women suffering non-cancerous gynaecological disorders, such as myomas, adenomyosis (endometriosis of the uterus), niches (caesarean scar defects) or congenital uterine abnormalities. Gynaecologist Professor Judith Huirne leads the clinic – but has greater aspirations.
This, Dr. Taylor says, stems from a lack of awareness in the medical community and among the public. “Often, women have bowel or bladder issues related to endometriosis because it affects all the surrounding organs,” he says. “And I can't tell you the number of people who have been sent to a gastroenterologist and had a colonoscopy or seen a urologist and had a cystoscopy rather than to an OB/GYN to get their endometriosis diagnosed and treated. When the pain is cyclic, coming mostly around the menses, physicians should first think of endometriosis. Symptoms that occur primarily at menses are not typical of most primary bowel or bladder problems.”
“Similarly, patients have been sent to a psychiatrist and been told, ‘You need to treat this anxiety. You'll calm down, and you won't be worried about that pain,’” Dr. Taylor adds. “This is incorrect. Endometriosis causes pain, but the endometriosis is also causing these changes in the brain.”
Q: Is there a path to a quicker diagnosis?
If menstrual cramps are getting more painful, that is not normal. Cyclic pain that is progressive over time is almost always endometriosis
Hugh Taylor
There isn’t yet a simple test to diagnose endometriosis. While certain symptoms like pelvic pain may point to endometriosis, the only way to know for sure is to conduct a laparoscopic surgical procedure in which a small telescope is inserted inside the abdomen through the belly button to look for endometrial tissue on the reproductive organs, intestines, or other surfaces. And unless the disease is particularly bad, endometrial tissue will not be visible on any imaging tests.
“But I think diagnosis can be very simple if you focus on a woman’s symptoms and history, especially if a woman’s pain worsens over time. Endometriosis is a progressive disease. Your first period at age 12 might set the baseline for what your periods will feel like in terms of pain. If menstrual cramps are getting more painful, that is not normal,” Dr. Taylor says. “Cyclic pain that is progressive over time is almost always endometriosis.”
Q: How can endometriosis treatment be improved?
If a woman has classic endometriosis symptoms, such as painful periods, Dr. Taylor says there is no need for surgery to make a diagnosis. The first step would be hormonal birth control, which can help with symptoms by stopping menstruation. Other options, such as the use of progestin, involve altering the hormones that cause the growth of the endometrium and the spread of these cells within the abdomen.
Unfortunately, many endometriosis treatments are hormonal, so they can have impacts far beyond the condition—for instance, they can cause menopausal symptoms. What’s more, these treatments are not specific to endometriosis, and they all prevent fertility, Dr. Taylor explains.
Surgery to treat endometriosis should only be considered if hormonal treatments do not work, he says, adding that laparoscopic excision surgery is a promising option. Dr. Taylor notes that the benefit of excision surgery is that the endometrial tissue is completely removed and not just destroyed. “Sometimes, the diseased tissue goes very deep, and if simply destroyed from the surface, one may not have treated the full depth of the endometriosis lesion,” he says. “Excision ensures that the full lesion is removed.”
Q: What do you hope changes in the public perception of endometriosis?
Ultimately, Dr. Taylor says he hopes the medical community begins to see the bigger picture regarding endometriosis. “We need to put everything into context and not get distracted by other symptoms. Listen to patients. If a woman has cyclic pelvic pain, it's probably endometriosis. Don't be distracted. All of the diffuse signs and symptoms that often accompany endometriosis are not unrelated. They're part of the manifestation of the disease. Let's look at the whole body and all the issues caused by endometriosis.”
Source: Yale Medicine; by Carrie MacMillan
25.08.2023










