Article • Women's health
Benign gynaecology specialist centres are needed
The recently opened Uterine Repair Center (URC) in VUmc (Amsterdam) serves women suffering non-cancerous gynaecological disorders, such as myomas, adenomyosis (endometriosis of the uterus), niches (caesarean scar defects) or congenital uterine abnormalities. Gynaecologist Professor Judith Huirne leads the clinic – but has greater aspirations.
Report: Madeleine van de Wouw

As a professor of benign gynecology, in her inaugural lecture in December 2017 she argued for the expansion of the number of benign centers for gynecology. In these specialist centers doctors can make better diagnoses using the latest diagnostic techniques, and perform treatments that are scientifically validated. ‘Research shows that one in three women has severe menstrual problems,’ Huirne points out. ‘Approximately 70% will postpone making a doctor’s appointment. When she finally does, she’s often told her complaints are “normal” – part of being a woman. But, severe menstrual complaints should be investigated. That’s also why these specialist centers are needed.’
The taboo is stronger than we realise
Judith Huirne
Many women dislike talking about their periods: ‘Through history, and in certain religions, there is a menstruation taboo. It’s seen as impure and therefore, for example, you can have no sexual intercourse. The taboo is stronger than we realise. Additionally, Dutch women don’t want to whine, so leave things as they are. Or they find a solution: one of my patients had such severe bleeding that she set an alarm twice a night to change her sanitary towels, or have to change the bed. This should not be acceptable. We need to increase women’s awareness, so they can recognise what’s normal and what isn’t.’
Take women seriously
According to Huirne, GPs and gynecologists also need to change their attitude with women who consult them with menstrual complaints. Often hormones are prescribed, but these suppress the symptoms and are not the solution. Also placing an IUD, or removing the uterus, are often a remedy, which does not work when a woman wants a child.
A lack of knowledge
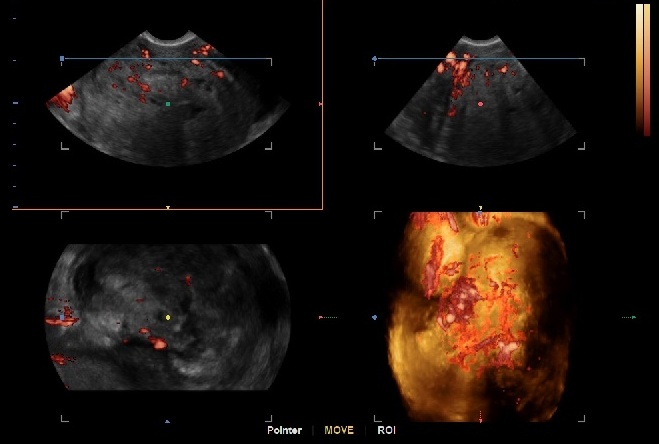
The main issue, Huirne believes, is lack of research into menstruation problems. ‘Myomas are often the cause. When you ignore them, they continue to grow, and minimally invasive treatment will no longer be possible. Myomas also can lead to fertility problems. In our clinic we see many women in their late 30s, early 40s, who want a baby and have tried to become pregnant for years. Often they were also in an unsuccessful IVF trajectory. Had they come before or after their first IVF, the problem could have been solved sooner.’ The first diagnoses can be done quite well in hospitals, Huirne says. ‘But you need expertise and specialisation to make every diagnosis and to discuss and perform all possible treatments and alternatives. Not every treatment is suitable for every patient. All those specialties are present in benign clinics.’
Adenomyosis
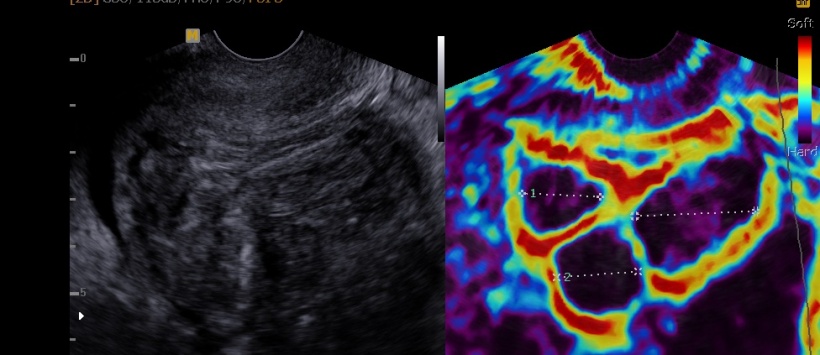
Alongside myomas, adenomyosis often causes menstrual problems. This form of endometriosis is located in the uterine wall between muscle tissue. Yet, this condition is not always recognised. ‘This also needs specialist clinics. There are new echo techniques that help to detect this condition. Also, better treatments should be developed and investigated – presently a new treatment is being investigated in the Uterine Repair Center.’
Caesarean section effects
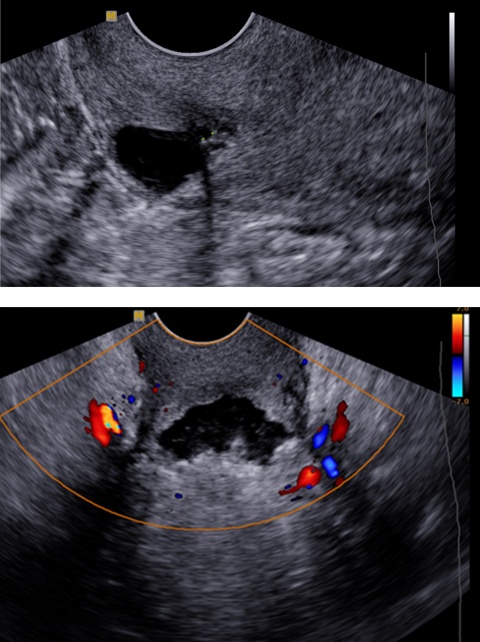
The Uterine Repair Center is the most specialised center in the Netherlands to treat patients with ‘niche complaints’. About 60% of women have a uterus defect after a caesarean. 25% of them even have large defects. The findings are that women with niches are three times more likely to develop abnormal bleeding after menstruation and an increased risk of fertility problems. ‘This also needs research, because niches can sometimes reduce the chance of a next pregnancy,’ Huirne points out. ‘Not every niche needs treatment. In our URC we determine whether womb repair is necessary, and examine the added value for women who want children.
Another task for benign centers is providing second opinions. If a treatment is non-beneficial, or the patient wonders whether the treatment is correct, the general practitioner can seek a second opinion. We often arrive at the same answer, and it resassures the patient if we propose the same treatment and refer her back to her own gynaecologist.’
Specialisation through centralisation
You can’t be a specialist by doing things now and then
Judith Huirne
How many centers are needed depends on how often a condition occurs. For Huirne one center is enough to treat caesarean section niches. For all other conditions five centers would be sufficient. ‘The Netherlands is a small country, so maybe you have to travel for an hour or so to find all the expertise you need in one place. In the center we can do research and treat niche resections and congenital abnormalities, like placing straps around the cervix via endoscopic surgery. That’s not a common procedure so it’s not desirable to do it in every hospital in the country. To become an expert, you need practice. You can’t be a specialist by doing things now and then. Through centralisation you can specialise, increase possibilities and can do much better research.’
Research is necessary
Huirne gained her doctorate on hormone regulation after IVF, but switched to benign gynecology. ‘I was surprised to learn there has been incredibly little research in this area. Only by chance we discovered how many women have problems with menstruation after a caesarean. How can that procedure be performed so often and we don’t observe what happens afterward? We know that over half the women between 40 and 50 years have myomas, but we have no clue as to why that is. As for cervical straps, mostly they are placed during pregnancy when there is already dilatation. That’s not always effective. We think for women with higher risk it is more effective if a band is applied before the next pregnancy. But that procedure is not suitable for everyone, because it involves endoscopic surgery, and the baby can only be born via a caesarean section. Our job is to find out whether it’s indeed effective and who is eligible.’
The VUmc currently runs several research lines in collaboration with gynecologists, radiologists and laboratory technicians. ‘We now supervise many PhD students who research myomas, adenomyosis and niches, etcetera. ‘Money is needed for all these studies, which is problematic. We want to do more research into the underlying cause of various problems, to develop more focused and effective treatments. Ultimately, this would bring down healthcare costs.’
Awareness
Huirne believes that, to function properly and take research and care to a higher level, more transparency is needed between doctors. ‘Tell your colleagues what you do, about any complications, or what you have encountered. Collaboration is important. Fortunately, in the Netherlands, we already often do so. ‘To make these clinics a success we need doctors to participate and refer patients to benign clinics. Colleagues in the clinics have to make standard agreements about researches and treatments. Everything must be discussed to give reliable information to the patients.’ Huirne stipulates that it doesn’t matter whether a doctor is male or female. ‘Doctors don’t need to have disorders themselves to know what they are talking about. The most important thing is that complaints are taken seriously and that per patient the best treatment is considered.’
The Uterine Repair Center has already been established, and will start a collaboration with AMC shortly. ‘I’m convinced that, if we continue to cooperate we can achieve so much when we offer good quality of healthcare and provide the right information in any way. There will be more centers. That is logical, since specialised clinics exist for all kinds of disorders, such as oncology. ‘Finally, we want to tell women to see a doctor! Both women and doctors must realise that severe or painful menstruations are not normal. Awareness. That’s where it all starts with.’
Profile:
Following a minor invasive surgery period at Ulleval University Hospital, Oslo, in 2007 gynaecologist Professor Judith Huirne MD joined VUmc Amsterdam, where she became professor of benign gynaecology in 2017. She now heads the gynaecology unit, specialising in minimally invasive treatments of uterine abnormalities including myomas (fibroids), adenomyosis (endometriosis of the uterus), niches (caesarean scars defects), congenital uterine abnormalities and cervical insufficiency. She has been involved in development of various new diagnostic techniques and treatments for uterine abnormalities, and founded the European expert group on uterine abnormalities. In 2017 the uterine recovery centre was founded.
05.03.2018










