Image source: Adobe Stock/SciePro
News • Tumour shrinking
"Downstaging" liver cancer before transplant improves outcomes
Treating liver cancer tumours to shrink them in order to allow the patient to qualify for a liver transplant leads to excellent 10-year post-transplant outcomes, according to new research.
The team from Mount Sinai published their findings in JAMA Surgery. The results validate current national policies around transplant eligibility.
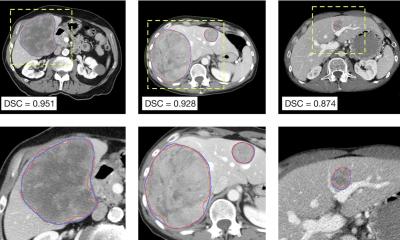
Selection of patients with hepatocellular carcinoma (HCC), the most common form of liver cancer, for transplant has been guided for more than two decades by standards known as the Milan criteria. The Milan criteria state that transplantation should be performed in those with a single tumour of five centimeters or less in diameter or three tumours that are each three centimeters or less in diameter, have no macrovascular invasion, and no metastasis. Over time, the rising incidence of HCC and mortality rates in the United States have led to refinements to the selection policy, shifting the focus to guidelines that also incorporate tumour biology, response to bridging therapies, and waiting times for patients within and beyond the Milan criteria.
Our study represents a solid confirmation that HCC patients effectively downstaged to Milan criteria have an outstanding median survival of 10 years, thus providing the rationale to adopt this policy on a global basis
Josep Llovet
One aspect of the current criteria is known as downstaging: the process of applying liver directed therapy to tumours too big for the Milan criteria with the hope of reducing them to the suggested size. Downstaging is now an option in selecting suitable liver transplant candidates with initial tumours that exceed the criteria. However, liver cancer can recur after transplantation, either within the liver or outside of the liver. The treatment options of patients who have recurrence post transplantation is limited and prognosis is poor.
In this cohort study, a retrospective multicenter analysis of prospectively collected data was conducted for 2,645 adults who had undergone liver transplant for HCC at five U.S. academic medical centers between January 2001 and December 2015. The analysis was performed from May 2019 through June 2021. Outcomes of 341 patients whose disease was downstaged to fit within the Milan criteria were compared with those in 2,122 patients whose disease always fit within the criteria and 182 patients whose disease was not downstaged.
The 10-year post-transplant survival and recurrence rates were, respectively, 52.1 percent and 20.6 percent among those whose disease was downstaged; 61.5 percent and 13.3 percent in those always within the criteria; and 43.3 percent and 41.1 percent in those whose disease was not downstaged. “Our study validates national policy on downstaging prior to transplantation and shows the clear utility benefit for transplantation prioritization decision-making,” said Parissa Tabrizian, MD, co-lead author on the study and Associate Professor of Surgery at the Icahn School of Medicine at Mount Sinai. “These results can increase the level of recommendations for the downstaging policy on a global basis. It also demonstrates that surgical management of HCC recurrence after transplantation is associated with improved survival in well-selected patients and should be pursued. The study also supports expanding the policy of downstaging applied to guidelines in Europe and Asia.”
“Our study represents a solid confirmation that HCC patients effectively downstaged to Milan criteria have an outstanding median survival of 10 years, thus providing the rationale to adopt this policy on a global basis,” said Josep Llovet, MD, PhD, co-lead author on the study and Founder and Director of the Liver Cancer Program at Mount Sinai Health System. “With this study clinical practice guidelines of management of HCC can recommend our approach with an acceptable level of evidence.”
Source: Mount Sinai Health System
25.07.2022