Source: Shutterstock/Lightspring
Article • Wishlist
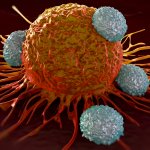
Cancer prevention scrutinised
The latest study by the German Society for Haematology and Oncology (DGHO), ‘Prognosis for population-based morbidity for common cancers in Germany – impact on provision’ has made it clear that due to demographic developments in Germany and to medical advances in oncology, the requirements for cancer patients’ care are ever more diverse.
The increase in newly diagnosed cancer patients is likely to be around 10%. The number of people living with cancer and those cancer patients with chronic concomitant diseases will also increase significantly. The current figures revealed in the study suggest important conclusions for the country’s health politics.

Source: DGHO/Wandelt
For its study, Germany’s DGHO used different data sources, such as population registers and epidemiology cancer registers. It shows the predicted development of important parameters such as the number of newly diagnosed cancers and prevalence right down to regional level. ‘This enables very precise and differentiated statements on trends in cancer care in this country, which would otherwise not be that obvious,’ emphasised Professor Carsten Bokemeyer MD, Chairman of the DGHO.
The analysis only included audited cases, meaning that an overestimation of the initial figures is unlikely. According to estimates from the Robert Koch Institute, not all federal German states achieved the required reporting rates of 90% for the entities in 2014. It is therefore assumed that the figures for incidence as well as for the resulting prevalence are likely to be slightly higher than those stated in the report. Possible regional developments not caused by age structure and gender ratio were disregarded. New therapy approaches and innovative treatments that will lead to an improvement of the survival rate were also disregarded.
The most important results of the study were summarised concisely by Professor Wolfgang Hoffmann MD, who conducted the study. All projections are based on the demographic development of the German population. It is assumed that the country’s overall population will increase by around 1.3 million people between 2014 and 2025.
However, this will not happen evenly across all age groups. In fact, it is expected that the number of men and women aged 60 and above will increase by 21% and 15% respectively. Among men and women aged 80 and above, the increase is likely to be as much as 51% and 26% respectively. In absolute figures this is an increase of 1.6 million in 2025 compared to 2014. This goes hand in hand with a decrease in the single digit percentage range of the number of those aged between 10 and 59 of both genders.
It’s clear that the requirement for specialists over the next few years will grow due to the rising incidence and increasingly complex treatments
Maike de Wit
Age-related tumours will therefore become more common, and the complexity of cancer cases will increase for many patients. Looking at the most common cancers, the following prognosis can be made: The number of newly diagnosed cancers between 2014 and 2025 will likely increase by 10%, meaning that, in 2025, there will be more than 520,000 cases per year. For men, the biggest increase will be seen for prostate cancer and, for women, breast cancer will increase the most with old age. The 10-year prevalence of cancers will increase considerably between 2014 and 2025. An increase of around 8%, to almost three million patients, is expected.
The number of patients who suffer from at least one further chronic disease alongside their cancer is also expected to rise significantly. The study used the figures for cancer patients who also suffer from diabetes mellitus, chronic obstructive pulmonary disease (COPD), coronary heart disease, obesity, renal insufficiency or dementia at the same time for these calculations.
An improvement in care structures in rural regions is urgently required. Clearly, the number of older people living in rural areas will be disproportionate. Against this background it is to be expected that the requirements for specialist cancer treatment will increase. ‘It’s clear that the requirement for specialists over the next few years will grow due to the rising incidence and increasingly complex treatments.
‘We need to establish structures of provision that make the competence in specialised centres available comprehensively, if we don’t want to risk entire regions, or the aged, being left behind when it comes to cancer care,’ emphasised Professor Maike de Wit MD, of the Working Group for Haematologists and Oncologists in the Hospital e.V. (ADHOK). It would therefore be beneficial to see a further delegation of medical services and more efforts towards the implementation of Medical Care Centres (MVZ) in community hospitals.
Recommended article
Article • Therapeutic progress
Cancer: riding the wave of innovation
In haematology and medical oncology, there is always something new. However, the increasing stratification of cancer therapies presents an enormous challenge for clinical research. Tumour cells – those altered genetically by mutation and thus ought to be recognised by the immune system and destroyed – manage to apply diverse molecular tricks to avoid attack by the immune system. Thus, they…
It also became clear that high quality, outpatient cancer care must be made available comprehensively. ‘Comprehensive and optimal cancer care requires concepts which integrate cancer care,’ said Ingo Tamm MD, of the Professional Association of Haematologists and Oncologists in Germany e.V. (BNHO). The increasing cancer prevalence is a particular challenge. ‘Very good treatment options for chronic myeloid leukaemia (CML), for instance, have led to a greatly increased pre-valence of these patients – 20,000 and more in the next few years. We must provide outpatient oral treatment for them in the best possible way,’ Tamm said.
The increase of comorbidities leads to a more complex situation for outpatient care. Cancer patients must be treated more individually, must be monitored more closely with regards to recurrences and, in the advanced stages of the disease, must be given the best possible palliative care. With this complexity in cancer treatment and provision, haematologists and oncologists working in outpatient care are playing key roles alongside specialist cancer centres. Therefore, it is important that these specialists are supported by specialised cancer nurses, palliative care teams, as well as trained general practitioners. Telemedical care should also be extended.
‘The results of the DGHO study are not least an appeal to all of us and to politicians to advance cancer prevention,’ Bokemeyer emphasised in conclusion. ‘Cancer risk increases significantly with age, but it is not unalterable.’
Source: Prognosis of population-based morbidity for common cancers across German and the impact on provision. DGHO position paper on the challenges caused by demographic changes for future requirements in oncological care in Germany
22.08.2019





