Breast surgeons have endorsed ultrasound for decades
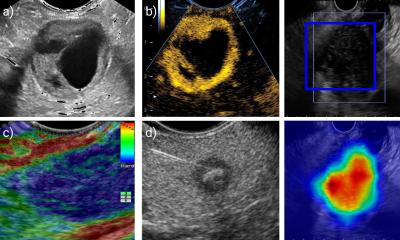
Ultrasound may be used during breast conservation surgery, to locate tumour lesions or to place localising wires; it can also guide a lumpectomy and perform a specimen exam to ensure a lesion has been excised and to evaluate surgical margins
Its versatility as a guidance tool also extends to cyst aspiration, core needle biopsy, needle localisation, and placement of brachytherapy devices. Intra-operative ultrasound does not require the sophisticated equipment needed for diagnostic ultrasound because it functions as a guidance tool during surgery.
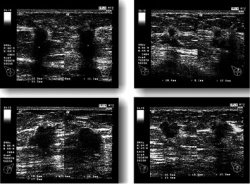
More breast surgeons in Europe use ultrasound than those in North America. The American Society of Breast Surgeons (ACBrS) estimates that 60-70% of its 3,000 members perform ultrasound, but the society has only certified 300 members. However, according to Dr Sara Fredrickson, ASBrS Chair of breast imaging technologies, ‘More and more surgeons are recognising the value of utilising ultrasound in their practices. Diagnostic ultrasound can evaluate palpable abnormalities, mammographic abnormalities, breast pain, and nipple discharge.’
She also pointed to real benefits for patients. ‘A patient with a palpable mass can have a physical exam and an ultrasound in the same visit. This eliminates the need to make an appointment for the exam at a radiology department. If the surgeon identifies a cyst from ultrasound images, the cyst can be aspirated in the surgeon’s office. This is just one example, but it saves the patient time and lessens the patient’s anxiety. It is also more cost efficient.’
For many years, women undergoing breast conservation surgery for early stage breast cancer who had a positive sentinel lymph node biopsy also had axillary lymph node dissection. These recommended guidelines changed dramatically in 2010 due to results from the American College of Surgeons Oncology Group (ASCOG) Z0011 randomised prospective clinical trial. This compared outcomes of nearly 900 women who had a cancerous sentinel lymph node. Cancer recurrence was the same for women who only had a sentinel node dissection and those who had multiple lymph node dissection. The women had been followed for a median of six years when Dr Armando E Giuliano, the trial’s principal investigator, announced the results. (Annals of Surgery, Vol.252:3, pp.426-433, September 2010).
Thus for a segment of women with breast cancer whose surgeons follow the ASCOG Z0011study recommendations there is less long-term pain and underarm discomfort and a lower risk of developing lymphoedema. Costs of surgery and follow-up care are also lower.
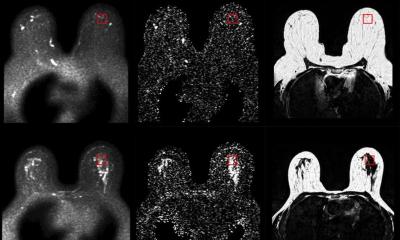
In 2011, researchers from Maidstone Hospital in the United Kingdom determined that contrast-enhanced ultrasound could identify and localise sentinel lymph nodes prior to breast biopsy. This capability offers the potential to produce more accurate biopsies and allow a patient’s cancer and positive lymph nodes to be removed in a single surgery. The study’s lead investigator Dr Ali R Sever, at the Department of Radiology, said that as many as 35% of patients require additional surgery following sentinel lymph node excision biopsy. (AJR, Vol. 196:2, pp251-256, Feb. 2011). Findings from a study at the Mayo Clinic in Rochester, Minnesota, recently presented at the American Society of Breast Surgeons (ASBrS) annual meeting, reinforced the role of ultrasound as a precise, non-invasive diagnostic tool to identify axillary metastases. The study showed that only 2% of patients with negative axillary might need to be considered for additional dissection after sentinel lymph node biopsy. (J Am Coll Surg. Article in Press 26 April 2013.)
‘Applications for pre-operative auxiliary ultrasound (AUS) have been increasing over the last several years. Although its utility has not been universally accepted by breast surgeons, more studies are now being published about its benefits,’ said co-presenter Dr Irada Ibrahim-Zada PhD, now affiliated with the University of Arizona’s Department of Surgery. ‘Our study, involving 1,140 women, confirms the very high sensitivity of pre-operative AUS as a diagnostic tool to detect lymph node metastasis. Its time has come. It can decrease surgery time, which contributes to better use of operating suites. It can eliminate frozen-section analysis, which also reduces treatment costs. And some breast cancer patients benefit by being able to avoid invasive surgical procedures.’ Additionally, at RSNA 2012 Finnish researchers from Kuopio University Hospital reported that ultrasound-guided axillary lymph node core-needle biopsy is a more effective diagnostic procedure than fine-needle aspiration in the pre-operative staging of invasive breast cancer patients. The prospective, comparative study of the accuracy of both procedures involved 120 women, and was the first such study to do so, according to presenter Dr Suvi Raultiainen.
As breast cancer treatment becomes individualised with the tendency to avoid treatment that may not benefit a specific patient, ultrasound is expected to play an even more important role.
05.07.2013