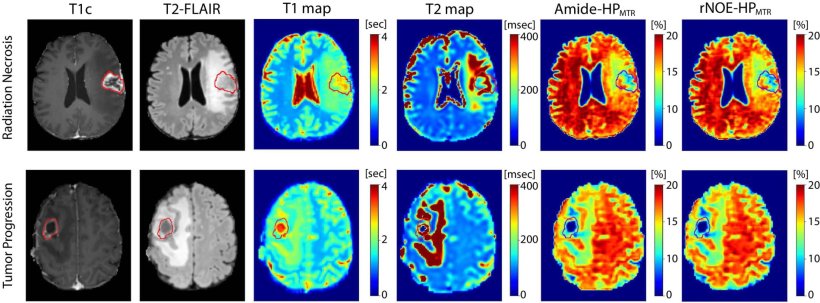
Image source: Bhatti NB, Young D, Lam WW et al.: Attention-Guided Deep Learning of Chemical Exchange Saturation Transfer Magnetic Resonance Imaging to Differentiate Between Tumor Progression and Radiation Necrosis in Brain Metastasis; International Journal of Radiation Oncology, Biology, Physics 2025 (CC BY 4.0)
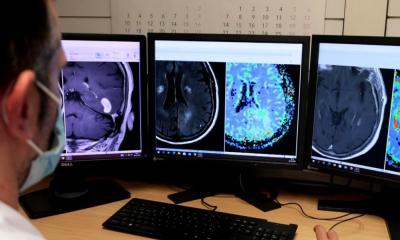
News • Differentiation after radiotherapy
Brain tumour or radiation necrosis? AI can tell them apart
While targeted radiation can be an effective treatment for brain tumours, subsequent potential necrosis of the treated areas can be hard to distinguish from the tumours on a standard MRI.
A new study led by a York University professor in the Lassonde School of Engineering found that a novel AI-based method is better able to distinguish between the two types of lesions on advanced MRI than the human eye alone, a discovery that could help clinicians more accurately identify and treat the issues.

Image source: York University
“The study shows, for the first time, that novel attention-guided AI methods coupled with advanced MRI can differentiate, with high accuracy, between tumour progression and radiation necrosis in patients with brain metastasis treated with stereotactic radiosurgery,” says York Research Chair Ali Sadeghi-Naini, senior author of the paper and associate professor of biomedical engineering and computer science. “Timely differentiation between tumour progression and radiation necrosis after radiotherapy in brain tumours is a crucial challenge in cancer centers, since these two conditions require quite different treatment approaches.”
The study was conducted in close collaboration with imaging scientists, neuro-oncologists and neuro-radiologists at Sunnybrook Health Sciences Centre using data acquired from more than 90 cancer patients whose original cancer had metastasized to the brain.
Sadeghi-Naini says the incidence of brain metastasis is rising as treatments improve and survival rates increase. Stereotactic radiosurgery (SRS), where a concentrated doses of radiation are applied to the cancer lesions only, is effective at controlling the tumours. In up to 30% of cases, SRS is not able to control the tumour and it continues to grow. Where it is successful, healthy brain tissue immediately surrounding the tumour may also die off, called brain radiation necrosis, and it can come with significant side effects.
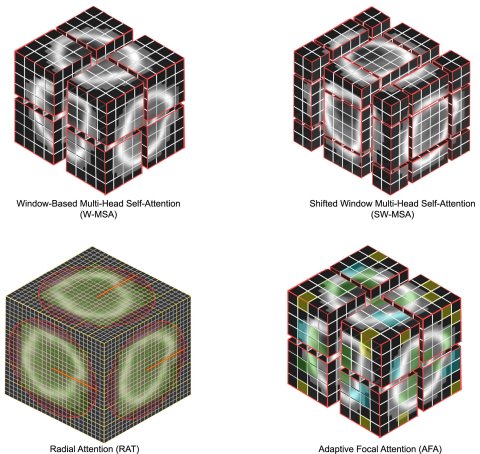
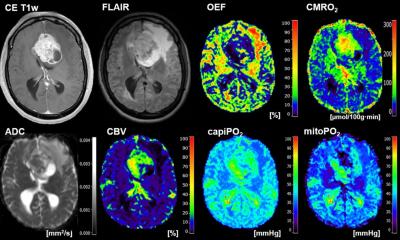
Image source: Bhatti NB, Young D, Lam WW et al.: Attention-Guided Deep Learning of Chemical Exchange Saturation Transfer Magnetic Resonance Imaging to Differentiate Between Tumor Progression and Radiation Necrosis in Brain Metastasis; International Journal of Radiation Oncology, Biology, Physics 2025 (CC BY 4.0)
Sadeghi-Naini and his colleagues introduced a 3D deep learning AI model with two advanced attention mechanisms to differentiate between tumour progression and radiation necrosis using a specialized MRI technique, called chemical exchange saturation transfer (CEST), and found that the AI was able to differentiate between the two conditions with over 85% accuracy. Sadeghi-Naini says with a standard MRI the two conditions are accurately diagnosed about 60% of the time, and with more advanced MRI techniques alone, the rate increases to about 70%.
“Differentiating tumour progression and radiation necrosis is very important — one needs more anti-cancer therapies and may need to be aggressively treated with more radiation, sometimes surgery. The other may require observation, anti-inflammatory drugs, so getting this right is crucial for patients.”
Source: York University
11.12.2025