News • Beyond PSA monitoring
New prostate cancer risk model could better guide treatment
One of the biggest challenges in treating prostate cancer is distinguishing men who have aggressive and potentially lethal disease from men whose cancer is slow-growing and unlikely to metastasize.
These risk groups were developed decades ago and were optimized for what is called biochemical recurrence, which simply means that a man’s PSA level rises again sometime after treatment
Daniel Spratt
For years, prostate-specific antigen (PSA) level, cancer grade and tumor stage have been used to sort prostate cancer patients into risk groups established by the National Comprehensive Cancer Network. These risk groups help determine treatment course. But the longtime practice has shortcomings. “These risk groups were developed decades ago and were optimized for what is called biochemical recurrence, which simply means that a man’s PSA level rises again sometime after treatment,” says Daniel Spratt, M.D., associate chair of research and assistant professor in the Department of Radiation Oncology at Michigan Medicine. “It was not optimized for more meaningful outcomes like identifying which men will ultimately develop metastases or die of prostate cancer.” That means men with prostate cancer are being left behind in the era of precision medicine, Spratt says.
The good news? Technology has advanced to the point where genetic information derived from tissue biopsied at diagnosis can much more accurately predict which men have aggressive prostate cancer. A genomic classifier score is assigned based on tests run on 22 genes known to increase the risk of developing metastatic disease.
The bad news? There has been no way to integrate these new gene expression biomarker risk scores into the NCCN risk groups that have traditionally been used to guide treatment.
“So what we did is basically say: We’ve got a flawed model,” says Spratt. “We’ve got these new biomarkers, but we don’t really know how to integrate them. Let’s see if we can merge them together to create a new, integrated system that is simple and easy to use, and standardize the use of these biomarkers.” The study was reported in the Journal of Clinical Oncology.
New reporting methods
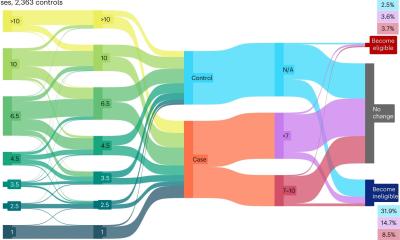
Four multicenter, retrospective cohorts of nearly 7,000 men, all of whom had gene expression biomarker scores, were used to design, test and validate a new model for assigning risk groups. Two new clinical-genomic systems were created: a simple three-tiered system and a more granular six-tiered system. When the researchers tested the new risk group models against conventional NCCN risk groups for the development of metastatic disease and death from prostate cancer, they found that the new clinical-genomic groups were much more accurate predictors than the traditional NCCN risk groups. The team also found some noticeable differences. “What our new system does is not only more accurately identify men who have either indolent disease or aggressive disease, but it reclassifies almost 67 percent of men, potentially changing recommendations for their treatment,” says Spratt.
Implications for care
This could radically change the way we perceive and treat localized prostate cancer
Daniel Spratt
For men with a lower-risk, slow-growing disease who are much more likely to die of something other than prostate cancer, active surveillance is typically recommended. Through careful monitoring of the condition, they are able to defer treatment. “It’s great because you spare the cost and side effects of treatment,” says Spratt. “However, in the community setting, only about 50 percent or less of men who we would normally say should go on active surveillance actually go on it. That’s because clinicians don’t have great confidence in the old NCCN risk grouping system.” This new system creates a much larger pool of low-risk men eligible for active surveillance, and it gives more accuracy and confidence to doctors prescribing treatment.
On the other hand, the new risk group classification also identifies a much larger pool of high-risk men who, if left untreated, are likely to die of prostate cancer. This group would receive more intensive treatment, possibly including radiation, hormone therapy or clinical trials. “This is similar to what the oncotype recurrence score is for breast cancer,” Spratt says. “Women who have a high oncotype score are told they have a large chance of absolute benefit from adding chemotherapy, while those with a low oncotype score may have a very small benefit — but the absolute benefit is so small, it’s not worth the side effects and cost of the therapy.” Spratt says this new clinical-genomic risk grouping system for prostate cancer is ready to be used today. “This could radically change the way we perceive and treat localized prostate cancer,” he says.
Source: Michigan Medicine - University of Michigan
20.02.2018