Prostate radiological
‘We need more feedback’
What you see is what you get - unfortunately, this doesn’t always apply in cancer imaging. Why is it that something which looks conspicuous on an image later turns out not to be a tumour? Why, on the other hand, are things overlooked that later turn out to be cancer? Pathological findings are extremely important to help improve diagnostic precision in radiology. Both disciplines therefore engage in an intensive dialogue at German Congress of Radiology in May.
Report: Karoline Laarmann

One focus of this interdisciplinary exchange was the diagnosis of prostate cancer. In this field, Dr Matthias C Röthke, Senior Consultant at the Department of Radiology at the German Cancer Research Centre, in Heidelberg, is among the leading imaging experts.
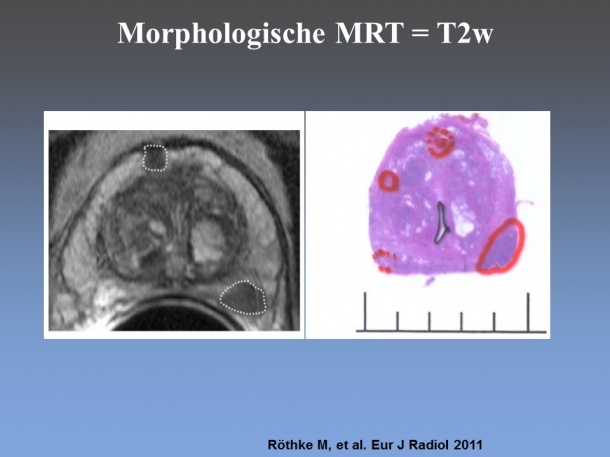
Currently, the procedure of choice for prostate imaging is multiparametric MRI, which supplements morphological image data with functional parameters. ‘The term functional basically refers to the diffusion behaviour in the tissue,’ Röthke explains. ‘Tumours are characterised by a high cell division rate. When you look at them under the microscope you see that the tissue consists of many large cell nuclei and little cytoplasm.
‘Accordingly, measurements carried out with diffusion weighted MRI show that the water molecules move around less freely in this type of tissue.’ A further, functional criterion, which is examined with the help of contrast media dynamics, is perfusion behaviour, because the perfusion patterns of tumours differ from those in healthy tissue.
If all available radiological measuring procedures are combined, this results in a sensitivity of 90%. ‘The diagnostic precision obviously also depends on the examiner,’ the radiologist admits. ‘If a procedure is carried out by an expert, the rate is higher than that achieved by a less experienced examiner. Unfortunately, there are as yet no certified radiologists who are specifically trained in prostate imaging, unlike those specialising in mammography. The referring urologists are making increasingly frequent demands for this further training because they are looking for reliable quality standards for prostate MRI procedures carried out by radiologists.’
Dr Röthke believes that organisational structures similar to those in place for the diagnosis of breast cancer are absolutely essential. This starts with the biopsy. The prostate is the only organ from which tissue samples are taken at random – with the help of transrectal ultrasound to assist with orientation – as part of the primary diagnosis. With all other organs, suspected lesions are precisely targeted under image guidance these days. ‘A prostate MRI should at least be carried out in patients whose primary, ultrasound-guided ten or twelve stent biopsy was negative, but whose PSA level continues to rise so that a possible lesion can be precisely targeted with a repeat biopsy,’ Röthke says.
His demands go beyond that. ‘What we need for prostate cancer are interdisciplinary case conferences as we know them from the field of breast cancer diagnostics. This would give us a quality forum where radiologists, urologists, radiotherapists and pathologists could exchange and update their knowledge. Such feedback discussions are currently usually carried out on an occasional and informal basis, whenever it fits into clinical routine. However, we need an official framework to achieve comprehensive and competent care for the imaging of prostate cancer.’
PROFILE:
Senior consultant Matthias C Röthke MD, Dipl.-Kfm. is primarily responsible for Urogenital Imaging within the Radiology Department at the German Cancer Research Centre (DKFZ) in Heidelberg. He studied medicine in Erlangen and Freiburg, completed his specialist training in Diagnostic Radiology at the University Hospital Tübingen and, in 2010, became a consultant at the DKFZ. Along with his membership of the Working Group for Uroradiology and Urogenital Diagnostics in the DRG, he is also a member of the Working Group for Prostate Imaging at the European Society of Urogenital Radiology (ESUR).
08.07.2015