Politics
Antibiotic resistance is a threat to global health
Within 15 years effective antibiotics will run out and, far from being an apocalyptic fantasy, a world in which common infections and minor injuries can kill is a very real possibility for the 21st Century. Geoff Sussman, one of the world’s foremost wound experts has warned that antibiotic resistance is posing the biggest single threat to global health.
Report: Mark Nicholls

Unless vigorous controls and restrictions are implemented in antibiotics use, he fears the consequences will be disastrous, with drugs that will no longer be effective against infections. Outlining his concerns to the annual meeting of the International Wound Infection Institute in London, Professor Sussman said: ‘Within the next 15 years we will run out of effective antibiotics and reach a situation where millions of people will die from simple infections because there is nothing to treat them. If action is not taken now, we will soon be back in pre-penicillin era.’
As Associate Professor in the Faculty of Medicine, Nursing and Health Science at Monash University in Melbourne, he highlighted the example of tuberculosis (TB), a disease thought to be under control a few years ago but which is now appearing as multi-resistant TB, which will not respond to any antibiotics. Over-use and misuse of antibiotics is driving the resistance, added Professor Sussman, who is also a senior clinician in wound clinic at Melbourne’s Austin Hospital.
‘We have misuse of low strength antibiotics on what are not really real infections,’ he said. ‘Here, bacteria can cope with low strengths and gain resistance to high strengths. Also, in surgery, it is not uncommon to use prophylaxis before an operation. That’s acceptable but some doctors continue using the antibiotic for another five days. That is no longer prophylactic, that is therapeutic and the overuse of the antibiotic.’
Bring in stricter controls
Overuse is common in General Practice with patients demanding antibiotics for colds and sore throats that are virus based and in this area of medicine he believes governments must implement stricter controls on where and who can prescribe some of these more potent antibiotics. ‘A bigger problem,’ he pointed out, ‘is in parts of the world like Asia where you do not need to see a doctor or get a prescription for antibiotics. You just walk into a store and buy them with no restriction at all.’
To help counter antibiotic resistance, Professor Sussman believes hospitals must work harder to control hospital-acquired infections, curb nosocomial infections with improved cleaning regimes and restrict strong antibiotics for use on only very serious infections. Few new antibiotics have been seen in 40 years because it is not economically viable for industry to develop drugs that patients will only use for a matter of days and he believes it should fall to governments to look at ways of funding research and developing new antibiotics.
Sussman also favoured a plan unveiled in a report by a UK government-appointed review team in May calling on the global pharmaceutical industry to pay for a £1.3 billion innovation fund to revitalise research into antibiotics. In return, guaranteed payments would be paid to companies that produce vitally needed new antibiotics. The move was devised in response to so few new antibiotics in development amid a global spread of resistant bacteria.
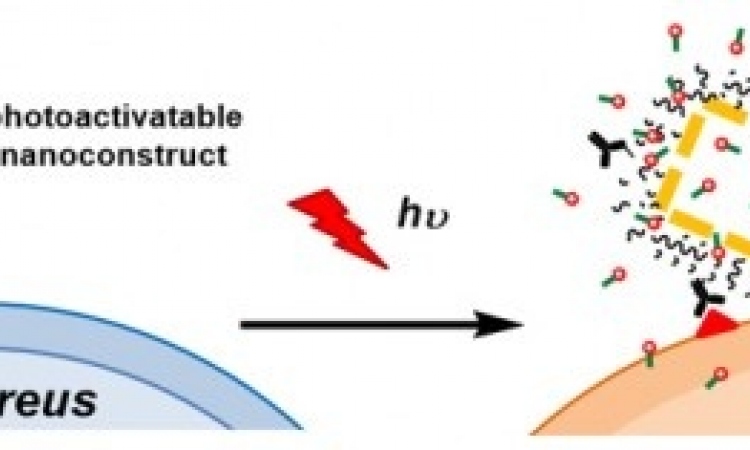
The professor also wants to see science develop innovative ways of attacking the bacterium other than antibiotics. ‘There are mechanisms that can attack bacterial cells and do not involve antibiotics. Those methods are then less likely to run into the problems of resistance.’
The urgency of the situation is dramatically underlined in the World Health Organisation document Antimicrobial resistance: global report on surveillance 2014. It states: ‘Antimicrobial resistance (AMR) threatens the effective prevention and treatment of an ever-increasing range of infections caused by bacteria, parasites, viruses and fungi. An increasing number of governments around the world are devoting efforts to a problem so serious that it threatens the achievements of modern medicine.‘A post-antibiotic era – in which common infections and minor injuries can kill – far from being an apocalyptic fantasy, is instead a very real possibility for the 21st Century.’
Areas taking a pro-active stance are Scandinavia and Australia, which has had therapeutic guidelines of antibiotic use for some years though many countries do not have them in place, he said. ‘But, there has to be concerted effort from the very top. ‘The World Health Organisation is already sending out the signals of how important it is and now governments, medical associations and agricultural organisations have to come together to fight this problem in a unified manner.’
PROFILE:
Geoff Sussman, who established the Wound Foundation of Australia, has been involved in research, clinical practice and teaching in the area of wound management for over 30 years. The inaugural Secretary of the World Union of Wound Healing Societies 2000-2004, he is also associate editor of the International Wound Journal and was awarded an OAM (Medal of the Order of Australia) in the Queen’s Birthday Honours in 2006 for his wound care work as a researcher, educator and clinician.
21.07.2015