Article • White matter hyperintensities
Uncovering the hidden part of the WMH iceberg
Cerebral white matter hyperintensities (WMH) can have a devastating impact on a patient’s life, yet knowledge of these lesions hasn’t really advanced over the past decades. Radiologists must learn to recognise these white spots in the brain and conventional imaging may just reveal the tip of the iceberg, a leading expert argued at the ECR Overture in March.
Report: Mélisande Rouger

Image source: Health Data Research UK
White matter hyperintensities of presumed vascular origin are the most common imaging feature of small vessel disease (SVD), which is a major cause of stroke and cognitive impairment. WMH play a role in both purely vascular dementia and its so-called mixed variant, for example in combination with Alzheimer’s disease.
WMH are the most studied small vessel lesions, which also comprise of small subcortical (or lacunar) strokes, lacunes and microbleeds. Yet there are still many unanswered questions about their appearance and behaviour, Professor Joanna Wardlaw, a consultant neuroradiologist with NHS Lothian in Edinburg, UK explained. ‘WMH can present in many different ways and that has partly masked the size of the problem,’ she said. What has been established is that the lesions are highly varied, they increase with age and are associated with risk factors such as hypertension, smoking, diabetes, lack of exercise, and additional socio-economic effects.
Not just a matter of age
Classifying WMH can be a bit of a puzzler for radiologists. ‘It’s quite hard to judge what should be normal in someone at a particular age,’ Wardlaw said. While the ideal state would obviously be a complete absence, there might be a bit of range, she ventured.
Recommended article
Article • T-2-weighted imaging
When the brain turns white
White matter on the brain is a difficult subject. Even the terminology is varied, making differential diagnosis complex. An understanding of prevalence and of the tools available to facilitate the diagnosis of individual diseases is important, Dr Gunther Fesl, radiologist at Praxis Radiologie Augsburg, explains.
Research has showed that WMH tend to start around the ventricles and later appear in deep white matter. ‘In the ages 50 to 69, you might expect most people to have only a thin periventricular line of WMH, and only one or two very small lesions elsewhere in the brain,’ she said. By the age of over 75-80, however, these numbers increase substantially and about 20% of people begin to have more numerous or even confluent WMH. ‘We still don’t understand the major reasons for the variation,’ she said. ‘Undoubtedly, these lesions are extremely important for future disease implications, so they shouldn’t just be dismissed as consequences of normal ageing.’
In the brain, many other things are white, apart from WMH
Joanna Wardlaw
For the longest time, researchers have studied lesions individually instead of as a totality – a mindset that may have delayed progress in the field, Wardlaw explained. ‘Combining lesions together gives much stronger indications of the impact of small vessel disease on several outcomes,’ she said. ‘Much stronger associations with smoking and cognitive impairment become evident, underlining the importance of considering these lesions together and not separately.’
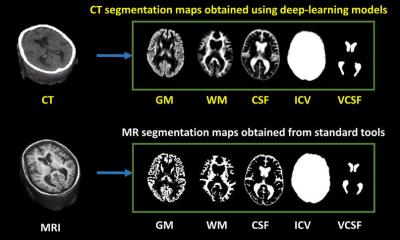
A number of visual scores have been developed to quantify WMH, which the expert regards as very useful tools to speed up burden of disease assessment. Computational measures have been developed more recently, but they are still a long way from being accurate, reliable, and fit for routine clinical use, according to Wardlaw. ‘Computational models increasingly use machine learning or deep learning, but none of them work perfectly,’ she said. For now, many of these methods simply pick up anything white in the brain – an overgeneralisation, according to the expert: ‘In the brain, many other things are white, apart from WMH.’
WMH shrinkage: technical error or actual phenomenon?
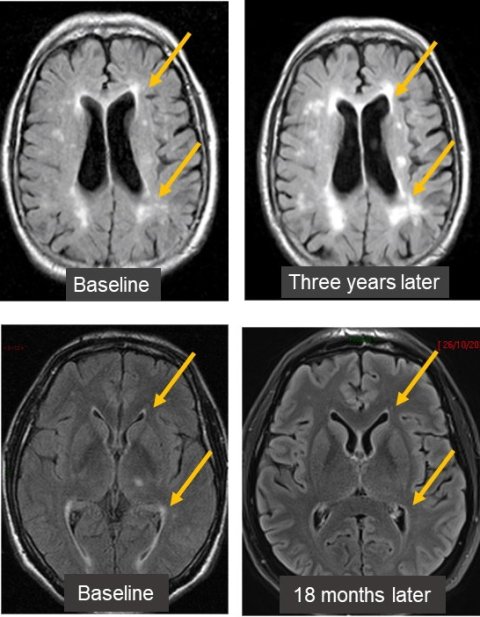
Image source: Prof Wardlaw
In most cases, differential diagnosis of WMH comes down to distinguishing between multiple sclerosis and lesions of vascular origin, Wardlaw reported. Most of the time, these lesions are easy to differentiate. A more controversial issue, she said, was the general belief that WMH tended to grow over time. ‘That’s the accepted wisdom, but it’s increasingly clear from MRI studies that some WMH – maybe up to 20% – can shrink in size,’ she said. ‘Shrinkage has been linked with patients having fewer recurrent neurological events, less cognitive decline and mobility impairment.’ This correlation suggests WMH shrinkage to be an actual phenomenon instead of just a technical error.
Wardlaw and her colleagues recently did a systematic analysis of all available evidence on WMH change and found that lesions do shrink more than is currently expected. ‘There’s a wide range of WMH change, but the analysis overall shows evidence of shrinkage across a wide range of populations,’ she said.
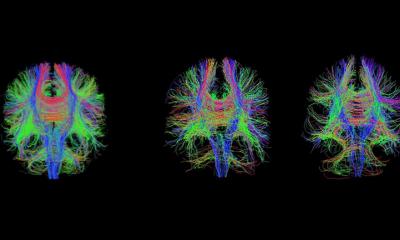
Another source of misjudgement is the so-called “normal appearing white matter” around the WMH, where the brain is actually not normal, Wardlaw cautioned: ‘If you look at parameters like blood-brain barrier leakage or white matter structure assessed using diffusion tensor measures, you’ll find these become increasingly abnormal as the WMH increase.’ What radiologists see as WMH on conventional MRI or CT is just the tip of the iceberg, she said. ‘You can create contours that show the increasing severity of these measures in so-called normal appearing white matter the closer you get to the WMH,’ she said.
Because WMH are white, they are often thought of as being ‘ischemic’, but this is probably too simplistic a way of looking at them, according to the expert. ‘There’s increasing evidence that blood-brain barrier failure is part of the mechanism underlying the formation of WMH. There’s also evidence that the small blood vessels get stiff and can’t increase blood flow when needed,’ she concluded.
Profile:
Professor Joanna Marguerite Wardlaw is a UK physician, radiologist, and academic specialising in neuroradiology of cerebrovascular diseases. Wardlaw worked as a junior doctor before specialising as a radiologist. She continues to practice medicine as an honorary consultant neuroradiologist with NHS Lothian. She has spent most of her academic career at the University of Edinburgh. Wardlaw is an expert in brain blood vessel diseases and neuroimaging. Her current research focuses on prevention, diagnosis, and treatment of strokes, particularly small vessel diseases.
19.05.2022