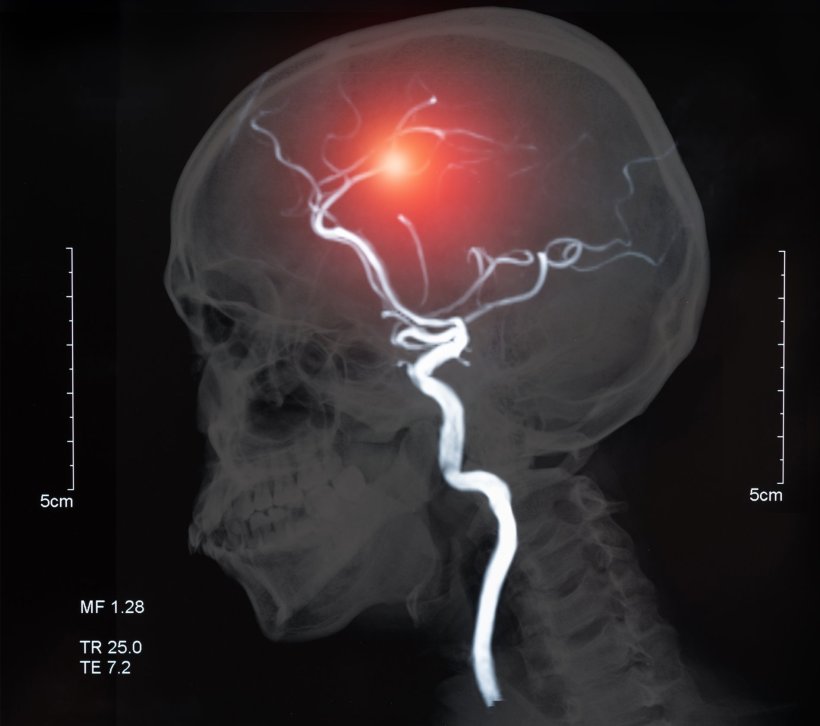
Image source: Adobe Stock/utah51
Article • Brain imaging
White matter hyperintensities: a valuable biomarker to assess mortality risk
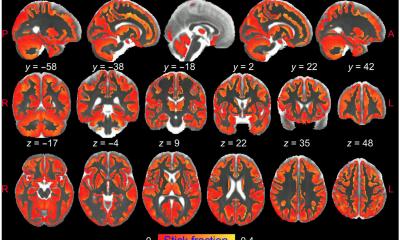
White matter hyperintensities (WMH) on the brain seen on MRI represent a biomarker associated with a 50/50 risk of death within five years after a first incident acute ischemic stroke (AIS) or transient ischemic attack (TIA).
Report: Cynthia E. Keen
Neurologists at the University of Bern have reported that prevalence and quantity of WMH are independently associated with mortality, and that patients with moderate or severe WMH and additional chronic covert brain infarctions (CBI) had the highest risk of death in a study published in the Journal of Neuroimaging.
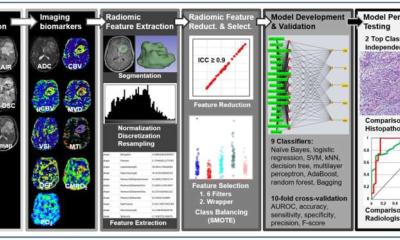
The findings are based on an analysis of mortality outcomes over 8,179 patient years of 2,236 consecutive patients who received treatment for first incident AIS or TIA at the comprehensive stroke centre of Bern University Hospital. The study investigated both the association of different phenotypes (observable physical properties), the quantity, and the locations of WMH and CBI with death, and also to determine if the presence of both improved predictability. WMH – subcortical lesions that appear as increased bright areas in the brain – are known from prior research to be associated with increased risk of stroke, Alzheimer’s disease and other dementias, and death. Little is known about the phenotypes of CBI.
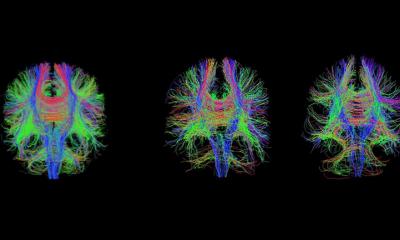
Easy and reliable assessment through routine imaging
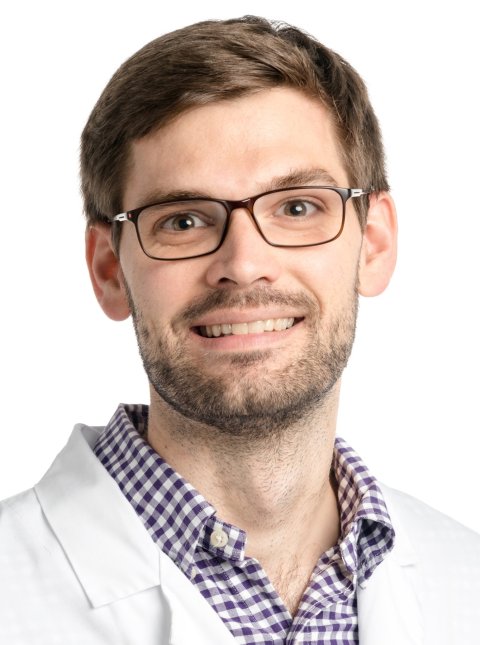
Image source: University of Bern
The researchers counted and mapped the location of CBIs, which included large subcortical infarcts, isolated grey matter lesions, combined grey and white matter lesions, and lacunes. They similarly counted and mapped the locations of WMH, as well as using the Age-Related White Matter Changes (ARWMC) scale to assess the severity of WMH. Using this classification scheme, they were able to differentiate between lesions that correspond to ischemic injury due to small-vessel disease and ischemic injury likely to be caused by embolism to the brain. All patients had undergone an MRI scan upon admittance to the hospital or within one week of diagnosis. Their median age was 71 years (range 59-80), and 57% were male. The patients were followed for a median of 4 years. The study did not track specific cause of death.
Principal investigator Thomas Raphael Meinel, MD, of Bern University Hospital’s Department of Neurology, and colleagues reported that patients without WMH had the least risk of dying, representing only 9% of deaths. The mortality was highest for patients with moderate or severe WMH (ARWMC 2 or 3) and CBI, at 37%, compared to 13% for patients with minimal WMH (ARWMC 0 or 1) and no evidence of CBI. Mortality was not associated with CBI phenotype, location, or count. The higher the ARWMC score representing increased WMH, the greater the risk seemed to be of dying. Forty-nine percent of patients with ARWMC 3 ratings died, compared to 29% with ARWMC 2, and 20% with ARWMC 1. Twenty-nine percent of patients with any CBI died, compared to 17% without any. ‘These brain frailty markers can be easily assessed without the need for advanced postprocessing,’ write the authors. ‘WMH can be reliably assessed on both routine 1.5 or 3 Tesla MRI and CT, and CBI on MRI. WMH are a more suitable surrogate marker than CBI for long-term mortality after stroke or TIA. Our study shows that 50% of patients with severe WMH have a life expectancy of five years after the event.’
As deadly as cancer – but more preventable
It is also important to note that not all WMH are due to vascular risk factors, but possibly due to a genetic mutation, and that these people may be living a very heart-healthy lifestyle
Thomas Meinel
‘It is appropriate to communicate with high-risk cardiovascular patients in a manner similar to communicating with oncology patients,’ Meinel tells Healthcare in Europe. ‘But unlike a cancer diagnosis, cardiovascular disease is highly preventable, and treatable by exercise, healthy diet, smoking cessation, blood pressure control, and medication. We tell patients with a high ARWMC score that there is a significant risk for stroke recurrence, and other major cardiovascular events including death. It is also important to note that not all WMH are due to vascular risk factors, but possibly due to a genetic mutation, and that these people may be living a very heart-healthy lifestyle,’ he adds. ‘At Inselspital Universitätsspital Bern, we provide a detailed tailored package of interventions for each patient. We follow-up with the high-risk patients to ensure that the risk factors are well controlled, and that the patient adheres to the optimal medication.’
Profile:
Thomas Raphael Meinel, MD, is an attending physician and group leader in the Stroke Center Bern of the Department of Neurology at Inselspital Universitätsspital Bern, Switzerland. His key research fields are stroke imaging, with an emphasis of covert brain infarction, futile interventions in endovascular stroke treatment, anticoagulation and stroke, and stroke prevention.
08.11.2022