UK researchers are working on a new MRI technique
UK researchers are working on a new MRI technique called hyperpolarised MRI – or Dynamic Nuclear Polarisation (DNP) – that can utilise more of the available nuclei than traditional MRI, helping to overcome some of its limitations by increasing sensitivity 10,000-fold or more. DNP is part of a longer-term aim to improve cancer mortality with the help of novel cancer imaging tools.
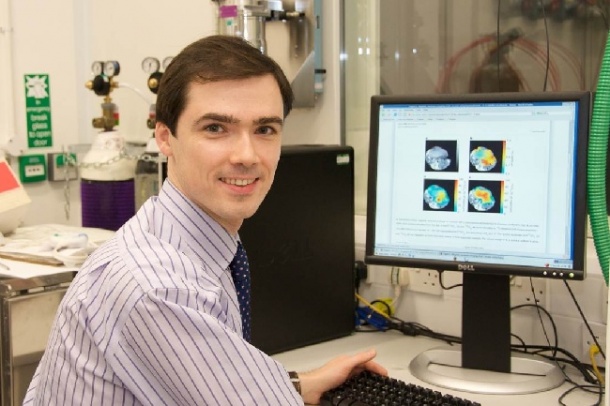
Dr Ferdia Gallagher, Cancer Research UK Clinician Scientist Fellow at CRUK Cambridge Research Institute & the University of Cambridge, said that MRI has the power to distinguish different molecules non-invasively within tumours. ‘The concentration of these can report on how metabolically active the cancer is and its rate of growth – both of which are important for predicting survival and for determining appropriate cancer therapy,’ said Dr Gallagher. ‘However, the great weakness of MRI is its lack of sensitivity: a typical MRI image utilises only a few nuclei in every million to produce the image that we are familiar with in radiology.’
His work on DNP, in collaboration with Professor Kevin Brindle of the CRUK Cambridge Research Institute, is focused on overcoming this problem and increasing sensitivity by considerable magnitude. The end result, he added, is a technique that can probe carbon metabolism non-invasively using MRI in patients; naturally occurring molecules can be labelled with a non-radioactive form of carbon, hyperpolarised using DNP, and then injected into an animal or patient.
‘The spatial distribution of the injected molecule can be imaged as well as the molecule(s) formed when the substrate is metabolised,’ he said. ‘This approach is similar to the use of a radiolabelled tracer in PET imaging but, unlike PET, the metabolites formed can be differentiated from the injected substrate using MRI, albeit with a lower sensitivity than with PET.’
The lead molecule is called pyruvate, a breakdown product of glucose, and both it and the lactate formed from it in a tumour can be imaged following intravenous administration. The first clinical trial involving this technique has taken place in the USA with prostate cancer patients and the UK team will be undertaking its first clinical trials in Cambridge shortly.
Dr Gallagher: ‘There are many unmet needs in clinical oncology where imaging is likely to play a role in helping patients of the future. For example, MRI can be used to give an early marker of successful response to treatment: patients who fail to respond to a drug therapy could be detected sooner using molecular imaging techniques, and then the patient could be quickly commenced on a more effective therapy. By probing specific and fundamental biological properties of tumours (such as how acidic the cancer is, or the surface expression of specific proteins), we may be able to stage cancers more easily and predict patient outcome more accurately in the future. The long term aim of molecular imaging in oncology is to improve cancer mortality with the help of novel oncological imaging tools.’
What continues to motivate Dr Gallagher and collaborators is that, while radiology has made great advances over the last 40 years in improving morphological imaging, the limits of anatomical resolution that can be achieved with conventional imaging methods such as CT and MRI has largely been reached. ‘We are therefore increasingly turning towards functional and molecular imaging techniques to provide new information about our cancer patients,’ he said. ‘The expectation is that these methods will be more sensitive and specific than morphological information alone. For example, hyperpolarised MRI could help us to reveal early changes in tumour metabolism following treatment, as well as predict the best form of treatment for patients.’
For patients – as medicine becomes more personalised and tailored to the individual - molecular imaging will play an increasingly important role in this by revealing some of a tumour’s molecular signature. ‘Functional and molecular imaging could also be used to detect tumours earlier,’ he added, ‘which is likely to have an impact on patient survival.’
PROFILE
Dr Ferdia Gallagher is CRUK Clinician Scientist Fellow, CRUK Cambridge Research Institute & University of Cambridge, and Honorary Consultant Radiologist at Addenbrooke’s Hospital. He studied medicine as an undergraduate at the University of Cambridge before completing clinical studies at the University of Oxford and training as a radiologist at Addenbrooke’s Hospital. His main area of interest is in developing molecular imaging techniques for oncological radiology and how these can be translated for humans. The focus of this work is to develop new molecular biomarkers to detect cancer, as well as methods to assess the early response of tumours to chemotherapy.
02.11.2012