News • DIY testing
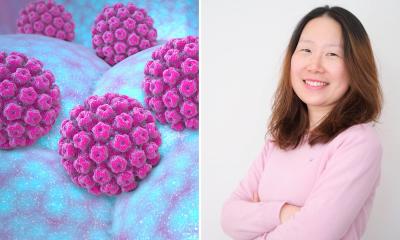
Self-sampling identifies twice as many women at risk of cervical cancer
Using self-sampling followed by HPV testing, more than twice as many women at risk of developing cervical cancer could be identified and offered preventive treatment.
This is shown by researchers at Uppsala University in the first randomised study in the world comparing two ways of identifying cervical cancer, published in the British Journal of Cancer. Cervical cancer screening has previously been based on cell sampling and cytology. This method initially reduced the number of cases of cervical cancer in Sweden substantially, but additional effects have been difficulty to achieve. This is due to the limited sensitivity of the method, and the fact that not all women attend screening. In the new study, researchers have compared today’s screening based on cytology and sampling by a midwife, with the woman taking a self-sample and submitting it for analysis of human papillomavirus, HPV, which is the cause of cervical cancer.
The study is based on 36,390 women between the ages of 30 and 49 who participated in the organised screening in Uppsala County, 2013–2015. These were divided into two groups: one group performed self-sampling for an HPV test, while the other group had a midwife take a cell sample for cytological analysis. Women who were HPV positive repeated the self-sampling after 4 months and those who were HPV positive in both of their tests were called in for gynaecological examination. During 18 months of follow-up, the number of women with severe cell changes was recorded for both groups.
The results show that self-sampling was received very positively. Of the women who were offered self-sampling, 47% opted to participate, compared with 39% among those who were offered regular cell sampling. Among the women who did self-sampling for HPV testing, more than twice as many with cell changes were found than among those who had a cytology analysis. Also, the time until diagnosis was shorter for those who did self-sampling.
Half as expensive, twice as effective
This is the first randomised study in the world that compares these two ways of identifying cervical cancer. By using self-sampling followed by HPV testing, more than twice as many women at risk of cervical cancer could be identified and offered preventive treatment. Screening based on self-sampling also makes it possible to reach women who have previously chosen not to participate and have a sample taken by a midwife.
Calculations of the health-economic consequences of self-sampling and HPV testing show that the total cost of cervical cancer screening could be halved, while still being twice as effective as current the method. Few changes in healthcare can simultaneously double the effectiveness and halve the cost. Screening based on self-sampling also makes it possible to reach women who have chosen not to participate in the cell sampling and take a sample in midwife.
Source: The Swedish Research Council
16.02.2018