© Naeblys – stock.adobe.com
News • Human papillomavirus infection
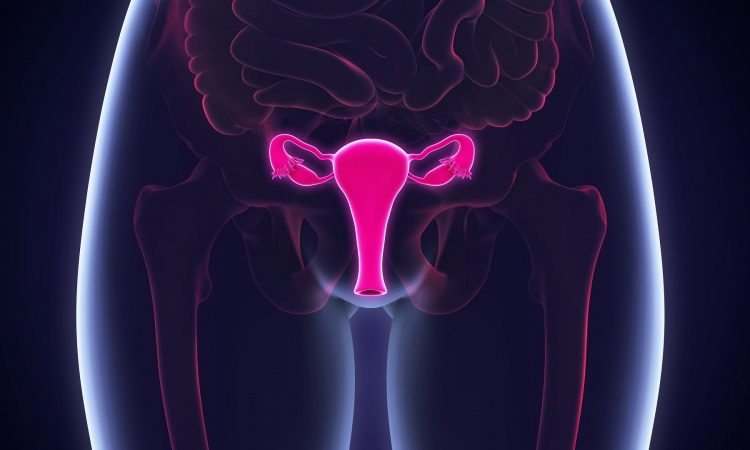
Cervical cancer: improved screening through HPV risk groups
Analyses of self-tests for human papillomavirus (HPV) can be used to divide HPV-positive women into three risk groups, according to a new study from Karolinska Institutet and Queen Mary University of London.
The results were published in PLOS Medicine. This method could be important for enhancing cervical cancer screening.

Image source: Karolinska Institutet; photo: private
The study is based on British women who were offered a self-test for HPV in a trial because they were overdue for their cervical cancer screening. "Self-testing for HPV has become an important component in cervical screening. It reaches women who would not otherwise participate," says Jiayao Lei, assistant professor at the Department of Medical Epidemiology and Biostatistics and Department of Clinical Science, Intervention and Technology, who is the lead author of the study.
The study, conducted in primary care centres in England, included 855 women with a positive HPV self-test, i.e. indicative of HPV infections, and had a subsequent clinician-sample. It was found that 71 of these women (8.3%) had the severe cervical precancer or cancer.
The researchers looked at the details of the HPV test results on self-sample and used a new method to assess the risk of severe cellular changes. The risk stratification is based on the variant of the HPV virus and the amount of virus (measured as the cycle threshold, Ct value) present in the self-test. Using this, they divided the women into three risk groups: high, medium and low risk. Women with HPV type 16 and a low Ct value (<30) had the highest risk of severe cervical precancer or cancer. "About 40% of women in our high-risk group had been diagnosed with the severe cervical precancer or cancer that requires treatment. Therefore, our recommendation for the future is that this group be referred directly for further investigation with colposcopy," says Jiayao Lei.
This could be particularly useful for cervical cancer screening in low- and middle-income countries, where resources are limited
Peter Sasieni
More than half of those who tested positive were in the low-risk group, with a 4% probability of being diagnosed with severe cervical precancer or cancer within 12 months. "We consider it would be safe for the low-risk group to be retested after 12 months; The moderate-risk group should be encouraged to get tested by clinicians," says the study’s senior author Peter Sasieni, Professor at Queen Mary University of London.
One of the major advantages of the new method is that the risk assessment can be done directly after the HPV self-test, without the need for further laboratory analyses. "This could be particularly useful for cervical cancer screening in low- and middle-income countries, where resources are limited", says Peter Sasieni.
The research team says that they will will perform a large-scale population studies based on self-tests in Sweden based on a different assay to test the feasibilities of including such risk stratification into the routine screening programs, supported by Swedish Cancer Society. They also want to investigate the predictive values of the current test results in combination with other markers for HPV-positive women.
Source: Karolinska Institutet
16.12.2024