Ploughing vigorously forward
The UK - In the 1990s, the nationally co-ordinated NHS Breast Screening Programme was already saving lives - a 21% fall in breast cancer mortality over the last decade and, with the cervical screening programme, this was viewed as among the best cancer screening programmes in the world. However, in that period, the country's cancer services, as a whole did not match up to those of other European countries.
In September 2000, the government published its NHS Cancer Plan, providing a long-term national strategy that heralded radical reform of cancer services, aimed at reducing mortality from cancers by at least 20% in people under 75 by 2010 (using 1995-97 figures as a baseline).
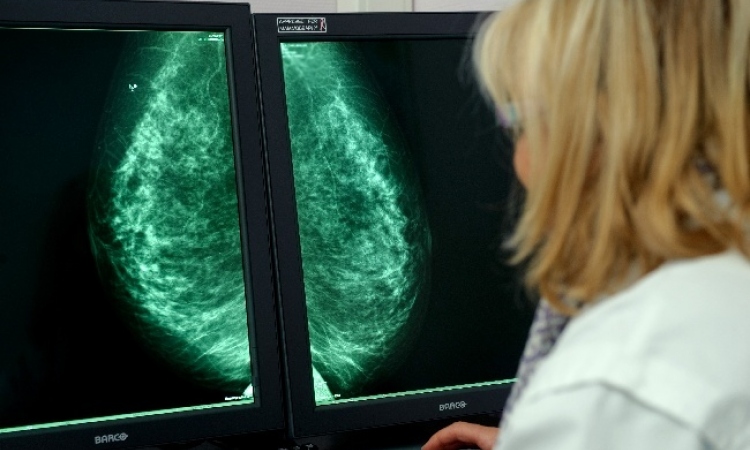
Between then and 2002 the country’s cancer death rate fell by 10.3%, which, by comparison of categories with results from other countries, indicated that Britain had achieved the world’s sharpest decrease in premature deaths from breast cancer and had made a substantial decrease in lung cancer deaths. In that period, 1.3 million women had been screened and 8,545 breast cancer cases were diagnosed. Now, new figures published in February 2004 have revealed that breast screening detected 9,848 cancers in 2002/03, over 13% more breast cancers detected by screening than in the previous year.
Because research has shown that two-view mammography could lead to a 42% increase in the detection of small cancers, this was also introduced to the programme, and itt is believed this produced the new rise in breast cancer detection. It involves taking two x-ray views of each breast during screening. By December 2003, 86% of local screening services carried out two-view mammographies. (England now has about 80 breast screening units at 87 sites - with some local breast screening programmes creating additional space by undertaking new building projects).
Breast cancer screening programmes were also extended and new programmes and technologies introduced - if proven lifesavers. Additionally, the NHS Breast Screening Programme was extended to include women aged 65-70 years, so that women aged 50-64, formerly invited for five screens, now receive two additional invitations for screening. An additional 400,000 women will be invited for screening annually by the end of 2004.
Screening staff - To remedy a dearth in radiographers, training places were doubled. Additionally, the Department of Health (DoH), partnered by the Society and College of Radiographers and the Royal College of Radiologists, developed a programme in which four new roles were created: assistant practitioner, state registered practitioner, advanced practitioner and consultant. Advanced practitioners are radiographers trained to take on some of the tasks of radiologists, i.e. interpreting X-rays and inserting marker wires to identify breast tumour locations. Trained assistant practitioners produce basic breast screening X-rays and can deliver basic radiotherapy to cancer patients.
The NHS reported that this role enhancement attracted more personnel to work for the NHS. By spring last year, 53 assistant practitioners and 158 advanced practitioners were employed and 28% of breast screening units were using assistant practitioners to help deliver the service.
Equipment - The DoH allocated £12 million to buy new breast screening equipment, which includes mobile screening units. Purchasing from 2000-2003 included 204 CT Scanners (164 replacements; 40 additional), 88 MRI scanners (51 replacements; 37 additional) and 91 linear accelerators (66 replacements; 25 additional), as well as 44 computers for radiotherapy planning, 23 simulators and over 600 devices for breast screening.
Patients - Under the NHS Cancer Plan, new information leaflets about screening were introduced to explain to patients the potential benefits and harm of screening programmes to help them base their decisions on evidence-based data (information overseen by the Advisory Committees on Breast and Cervical Screening and National Cancer Director). Since 2001, these have been included with the invitations women receive for breast (and cervical) screening.
Following publication of the government’s White Paper, ‘The new NHS - Modern, Dependable’, which guaranteed anyone with suspected cancer would see a specialist within two weeks of their general practitioner (GP) requesting urgent consultation, from April 1999 this applied to anyone with suspected breast cancer. It was reported that 96.9% of women with breast cancer now receive first treatments within a month of diagnosis. Ways of seeing non-urgent referrals within two weeks have also being investigated by the Cancer Services Collaborative ‘Improvement Partnership’ (CSC ‘IP’) breast group.
Rapid access (‘one stop’) clinics were also established for patients presenting common problems (including breast cancer symptoms) that might point to an underlying cancer. In addition, in some areas GPs can refer patients directly for diagnostic tests, bypassing the wait for a consultation.
To further streamline diagnoses, significant streamlining of diagnostic tests has also been a focus.
Peer reviews - To improve quality of care, assessments of cancer teams have been rigorous, and the value of peer reviews is generally acknowledged. A peer review steering group was established, closely linked to the shadow Commission for Healthcare Audit and Inspection (CHAI), and this summer a three-year peer review programme commenced.
01.07.2004