Article • Omics in cancer care
Personalizing laboratory medicine
To avoid adverse reactions, personalised laboratory medicine can help to predict a patient’s drug response. Investigations based on DNA and other omics technologies – e.g. genomics, transcriptomics, proteomics, metabolomics – along with microarray technologies, is making a particularly valuable contribution to cancer care, in which personalised approaches are becoming possible through molecular profiling.
Report: Mark Nicholls

Matthias Schwab, Professor and Chair of Clinical Pharmacology at the University of Tübingen, who also heads the Dr Margarete Fischer-Bosch Institute of Clinical Pharmacology in Stuttgart, Germany, believes that personalised laboratory medicine will have an increasingly important role in patient care over the next decade. However, he emphasises that the technique must be used in line with guidelines and recommendations – and where there is a clear consequence to the action, such as in drug selection or adjustment of dose.
This is particularly important in drugs that have a narrow therapeutic window, where the dose used is close to that which may result in drug-related toxicity. ‘Personalised laboratory medicine in healthcare is currently mostly implemented for treatment of oncology patients to avoid adverse drug reactions,’ he explained, adding that, in some areas, such as colorectal cancer, the approach is clearly defined – and where drugs (e.g. 5-Fluorouracil) to be used in clinical practice should be laboratory tested with a personalised medicine approach, for example to prevent haematoxicity and/or gastrointestinal side effects. ‘Personalised laboratory medicine is a crucial step in ensuring the dose is correct, that the treatment is correct, and matches the patient’s DNA, genetic profile and condition,’ Schwab emphasised. ‘Guidelines for healthcare implementation, that are regularly updated and publicly available, are there for doctors to select the right drug and adjust dose, or in some cases choose another drug. Personalised laboratory medicine also has value in research, by using consented information from a patient’s DNA to answer specific research questions.’
Recommended article
Article • Screening, early detection, treatment optimisation
AI techniques advancing oncology care
Cancer care and the treatment clinicians can offer patients is being increasingly enhanced by Artificial Intelligence (AI). The technology has a role in diagnosis, with algorithms trained to design and deliver patient care, can match patients to clinical trials they may benefit from, and even help predict outcomes and those at greatest risk.
Trends and applications in personalised laboratory medicine involve the application of newer drugs in cancer therapy, such as epidermal growth factor receptor (EGFR) inhibitors in lung cancer and can support genetic testing in therapy selection. With around 15 different drug targets (e.g. genes) and genetic variation, the technology can help clinicians select the right drug and dose in a process mostly conducted together with a pathologist using lung tissue.
Schwab feels this is the most promising application, but he foresees a move towards pre-emptive testing, not only in cases of drug failure after conventional cancer therapy, but also at the onset of therapy, where genetic information will be available when prescribing. When discussing personalised laboratory medicine in genomics, he emphasises that it is important to clearly define the genome variation. Germline DNA from individuals will ease this pre-emptive approach while, in cancer patients, personalised laboratory medicine must focus on DNA from the tumour. For patients with a tumour, where Next Generation Sequencing is currently mainly conducted only in cancer relapses, he suggests that, within the next decade, this will be a routine pre-emptive pharmacogenetic test.
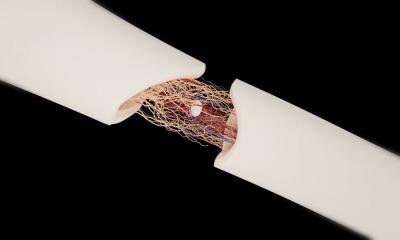
To Schwab, the benefits of personalised laboratory medicine are clear. ‘It’s about better treatment and selective drugs that will work if you carry a specific mutation, meaning patients will receive individualised treatment and not suffer toxicity.’ Such a medical approach promises more effective diagnostics with more effective and safer treatment, as well as faster recovery and restoration of health and improved cost effectiveness. ‘Personalised medicine in the genomics area is the future,’ he concluded, ‘but, in the next few years we will also talk about liquid biopsies because we can also use this information for epigenetic or metabolomic markers.’
Profile:
Matthias Schwab is Professor and Chair of Clinical Pharmacology and heads the Dr Margarete Fischer-Bosch Institute of Clinical Pharmacology in Stuttgart and the Department of Clinical Pharmacology, University Hospital, Tübingen, Germany. His major clinical and research activities are personalised medicine and pharmacogenomics with focus on cancer.
19.08.2021