Article • Precision oncology
Personalized health and genomics: Minimizing collateral damage
A solid diagnosis has always been the first step on any patient’s journey to health. However, diagnostic categories are necessarily oversimplifications. In the last decades, medical professionals and scientists have begun to uncover the true variability in patients’ physiological and biochemical make-up that is the principal cause for individual variations in the way diseases present themselves.
Report: Dr Christina Czeschik
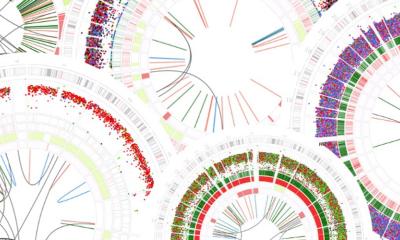
Image source: NCI Center for Cancer Research
A number of technologies have contributed to this massive increase in data and knowledge. In particular, radiology, histopathology and genetic sequencing are key fields in personalized medicine, and precision oncology is one of their top applications.
Cancer is extremely heterogeneous

Image source: Shutterstock/watchara
The different types of cancer (“lung cancer”, “breast cancer”) are in fact mixed bags of conditions that share only one feature: excessive cell growth. Chemotherapy and radiotherapy conventionally attack fast-growing and replicating cells. But as malignant and normal cells are still similar in many ways, such as their external structure and metabolic pathways, traditional cancer therapies are highly noxious to both normal and malignant cells. They cause a wide range of side effects, mostly in tissues with a naturally high proportion of healthy fast-growing cells, such as the gastrointestinal tract, bone marrow and skin. Their side effects may be as fatal as the underlying disease.
Thus, the holy grail of cancer medicine are therapies that are precisely targeted to eliminate malignant cells only. To develop such therapies requires a deep understanding of the cancer cell down to the molecular level.
Insights into the cancer cell: radiomics, histopathology, genomics
There are three main fields of medical science that contribute to an intimate knowledge of the workings of a cancer cell: radiology, histopathology and genetics/genomics. In recent decades, radiology has progressed from giving a rough orientation of a lesion’s spatial dimensions and internal structure to providing detailed information almost on a cellular level. In the newly developed field of radiomics or quantitative imaging, machine learning algorithms exploit subtle differences in signal strength that are invisible to the human eye. Similarly, histopathology has progressed from traditional H&E staining for visual examination under the microscope to far more sophisticated immunohistochemistry, using specific antibodies that bind to certain cell components. Information on a sub-visual level is being utilized as well, on secondarily digitized or primarily digitally acquired slides, employing machine learning methods to identify patterns predicting malignancy.
While radiology and histopathology are approaching the cancer cell from a macroscopic to a microscopic level, genetic sequencing is working its way up from a sub-microscopic level. High-throughput sequencing methods have all but replaced the conventional Sanger sequencing approach and have made it possible to sequence a cell’s whole genome in a matter of days or even hours. Massive genetic databases enable scientists to algorithmically identify pathogenic mutations within the overwhelming genetic variability of the human species.
Recommended article
Article • Innovation in intervention
The promise and reality about AI for interventional oncology
Is artificial intelligence (AI) technology ready to be utilized as a clinical tool by interventional oncologists? Not yet, but when it is, AI technology’s clinical impact may be as profound as advanced imaging is today, two leading experts agree.
Ideally, detailed knowledge about a cell population’s genetic aberrations helps to identify pathways that are instrumental for the growth of a specific tumour and can be inhibited with minimal collateral damage to the patient’s healthy cell populations. This so-called molecular profiling was implemented, among others, in the NIH-funded I-PREDICT trial. Of 83 patients with previously therapy-resistant tumours, 73 received an individual combinations of drugs matched to their respective molecular profile, with encouraging results regarding prolonged stable disease. To make results like these accessible to the medical community, there is now even a journal dedicated to personalized and precision oncology, Nature Precision Oncology (npj).
The principle of tailoring therapies to a patient’s genetic make-up is not limited to oncology: in pharmacogenomics, scientists investigate the influence of genetic variation on cellular pathways and thus the way that individual patients react to or metabolize drugs, finding out which drugs work best on a specific patient or subgroup of patients and which to avoid.
Challenges to conventional evidence-based medicine
However, personalized medicine poses a particular challenge to the way medical science has worked so far. In decades of evidence-based medicine and care, large randomized studies have become the gold standard of medical knowledge acquisition. Their goal is to evaluate the effects of a therapy (or other intervention) with optimum reliability and precision, eliminating bias, confounding factors and just plain coincidence as far as possible.
In the age of randomized controlled trials (RCTs), an intervention is only considered effective if there is a statistically significant difference in outcome still visible after averaging hundreds or thousands of patients. In this way, the RCT does not only eliminate coincidence but also the influence of individual genetic predispositions, unless the study population is chosen explicitly for a certain genetic trait. This, however, is possible only for the most frequent genetic variations. For example, breast and ovarian cancer patients are likely to profit from treatment with a PARP inhibitor only if they carry a BRCA-1 or BRCA-2 mutation. Such mutations are sufficiently frequent to include their carriers in large clinical studies. However, there are many more genes more subtly involved in cancer risk, and once we start considering not only single gene mutations but also combinations of mutations, things get infinitely more complex. As we know, there are hardly two people in the world sharing the exact same genetic make-up. Thus, the RCT might even be considered the antithesis of personalized medicine.
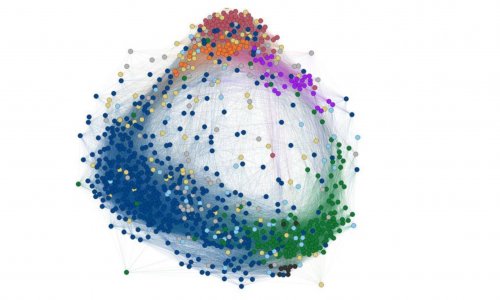
But the scientific community is already working on new solutions for patient populations as small as n=1. Experts of the US-based Translational Genomics Research Institute have coined the term “rapid learning systems” (RLS) for infrastructures that collect complex and real-world data on patients and their treatment outcomes. The goal of RLS is not, as in RCTs, to have as little heterogeneity in study populations as possible, but to record this heterogeneity as detailed as possible and use it to detect previously unknown associations between patient characteristics and treatment success.
In an even higher-level approach, not the efficacy of individually tailored drugs or drug combinations is investigated, but rather the quality of algorithms used to match a patient’s genetic profile to the optimum personalized drug regimen. Baby steps are being taken, for example, by comparing the performance of different machine learning algorithms in the prediction of efficacy and toxicity of chemo and radiotherapy. Meaningful progress will require massive amounts of precise clinical data as well as computing power, interdisciplinary collaboration and a further breaking down of barriers between medical, biological and computer sciences.
23.08.2021