Image source: Adobe Stock/Mladen
Article • Women's health
Osteoporosis and menopause: New measures to assess fracture risk
Bone fractures caused by osteoporosis are a common major global health risk. The International Osteoporosis Foundation (IOF) reports that one in three women over the age of 50 will sustain a potentially life-threatening fragility fracture in their remaining lifetimes.
Report: Cynthia E. Keen
Over 25.5 million women have osteoporosis, according to 2019 IOF estimated statistics.1 At least 23.8 million European Union (EU) residents are at high risk of osteoporotic fractures. Currently, the annual cost of osteoporosis-related fractures in Europe alone is estimated to be more than €56 billion for its population.2 Early diagnosis and proactive treatment to keep bones healthy, including prescription medication and lifestyle changes, has the potential to significantly reduce this risk and its financial burden.
Yet osteoporosis and osteopenia are among the most undiagnosed and untreated medical conditions, not only in Europe, but throughout the world. Governments and healthcare providers need to prepare for a skyrocketing number of cases, due in great part to an increasingly aging population, with Europe alone facing an estimated 25% increase in osteoporotic fractures between 2019 and 2034.3
Advocating for a public health strategy
In February 2023, the World Health Organization (WHO) and the European Society for Clinical and Economic Aspects of Osteoporosis, Osteoarthritis and Musculoskeletal Disease (ESCEO) signed an agreement to develop a strategic roadmap on bone health and aging, advocating for a public health strategy to prevent fractures among older people. This complements the IOF’s 2021 initiative to create an interactive Scorecard for Osteoporosis in Europe (SCORE) recording the burden of disease, policy framework, service provision, and service update of 29 EU countries.

Image source: Adobe Stock/SciePro
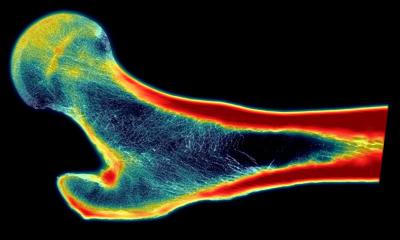
A bone mineral density (BMD) test is the best method to diagnose osteoporosis and assess bone strength. A dual-energy X-ray absorptiometry scan (DEXA), the most common and most versatile test, not only assesses bone strength, but also can provide a vertebral fracture assessment (VFA) to detect previously unrecognized spine fracture, a trabecular bone score (TBS) that assesses internal structure of bones in the spine at a microscopic level, full-length femur imaging to recognize thickening of the thigh bone that could lead to a stress fracture, and a hip structural analysis (HSA) to assess how the size, shape, and confirmation of hip bones can influence the strength of a hip. However, the cost of a BMD is prohibitive to many, and there are not enough DEXA scanners to meet global needs.
A free-of-charge Fracture Risk Assessment Tool (FRAX), created in 2008 by researchers at the University of Sheffield, calculates the absolute risk of fracture in 10 years independent of BMD assessment. This algorithm analyzes the clinical risk factors of age, current smoking, alcohol consumption, rheumatoid arthritis, family history of hip fracture, previous fragility fractures, and use of glucocorticoids.
New research from Asia
Current research studies are focusing on different indicators of fracture risk. A multi-institutional group of researchers from the Republic of Korea have validated a hypothesis that oral health is correlated with FRAX scores. Their study, published in Scientific Reports, is based on national survey data from over 2,300 Korean women over age 65 years.4 It statistically demonstrates that there are significant relationships between the number of teeth missing and FRAX 10-year probabilities of hip fracture risk.
As the tooth number in the elderly is an indicator of physical, mental, and social well-being, it can be considered as a potential parameter of fracture risk in the elder population
Seok Woo Hong, JunYeop Lee, Jeong-Hyun Kang
The researchers from Kangbuk Samsung Hospital in Seoul and Ajou University School of Medicine in Gyeonggi-Do explain that ‘losing teeth […] may lead to chewing difficulty, contributing to changes in food selection, malnutrition, and low bone and muscle mass. Good oral health influences the quality of life in a myriad way, including social interactions, communications, self-esteem, resilience, and adequate nutritional intake. As the tooth number in the elderly is an indicator of physical, mental, and social well-being, it can be considered as a potential parameter of fracture risk in the elder population.’ They advocate that dentists become aware of this association.
Another study by researchers at Shanghai General Hospital in China of over 1,200 post-menopausal women who sustained an osteoporotic bone fracture focused on the correlation between BMD and bone metabolic markers and levels of bone reabsorption.5 Bones consist primarily of calcium phosphate, a mineral compound that hardens the skeletal framework and type-1 collagen, a protein network that gives bone its tensile strength and framework. Bone marker testing helps determine if the rate of bone resorption is increasing, suggesting a potential bone disorder. Bone loss occurs when bone resorption occurs faster than the rate of bone formation.
The women included 1,008 who had sustained a single fracture and 231 who had a second fracture. The fracture sites included vertebrae, hip, pelvis, ankle, distal forearm and proximal humerus. None were caused by violent, high-energy impacts, bone metastases, or bone weakening from drug use.
Lead investigators Li You, MD, Xiaonan Zhu and colleagues determined that the higher the levels of the bone markers serum CTX and osteocalcin, which indicate bone resorption, the lower the BMD score. BMD scores were significantly lower for women who sustained second fractures than women who only sustained one. The researchers reported that women with high body mass index (BMI) and those not receiving anti-osteoporosis treatment were also at higher risk of sustaining a second fracture.
This fact is reinforced by the Brazilian Society of Rheumatology’s published endorsement of fracture risk assessment in the Revista da Associacao Medica Brasileira.6 The article states that almost nine million fractures annually occur worldwide due to osteoporosis, one occurring every three seconds. Additionally, if a person has already sustained an osteoporotic fracture, the risk of a second increases by 86%.
The Chinese researchers point out in menopause that although DEXA scans provide good estimates of bone tissue loss, the time elapsing between scans may be a period of high bone loss. Also, DEXA scans do not directly reflect bone metabolic status. They suggest that ’early recognition of the correlation between BMD and bone metabolic markers can better prevent further bone loss in women with post-menopausal fractures and thus reduce the risks of later fracture.’
References:
- International Osteoporosis Foundation: Epidemiology of osteoporosis and fragility fractures
- Kanis JA et al.: SCOPE 2021: a new scorecard for osteoporosis in Europe; Archives of Osteoporosis 2021
- Willers C et al.: Osteoporosis in Europe: a compendium of country-specific reports; Archives of Osteoporosis 2022
- Hong SW, Lee JY, Kang JH: Associations between oral health status and risk of fractures in elder adults; Scientific Reports 2023
- Zhu X et al.: Correlation between bone mineral density and bone metabolic markers in postmenopausal women with osteoporotic fractures at different C-terminal telopeptide of type 1 collagen levels: a retrospective analysis study; Menopause 2023
- Perez MO et al.: Osteoporosis and fracture risk assessment: improving outcomes in postmenopausal women; Revista da Associacao Medica Brasileira 2023
01.02.2024