Article • Differentiate and select
Myths and truths about antibiotics, antiseptics and vaccination
Sixty-two percent of Germans fear antibiotic resistance, according to a survey recently conducted by the German Federal Institute for Risk Assessment. ‘Patients colonised by multi-resistant pathogens are particularly scared.
Source: Shutterstock/amenic181
It’s true, however, that the spread of resistance genes and of multidrug-resistant organisms (MDROs), does correlate with the use of antibiotics: the higher the use of antibiotics, the faster the development of resistance
Mathias Pletz
But many of these fears are rooted in misunderstandings,’ explained Professor Mathias Pletz, Director of the Institute of Infection Medicine and Hospital Hygiene at University Hospital Jena, speaking at the Congress for Infectious Diseases and Tropical Medicine (KIT), held in Cologne, Germany. Many people believe the development of resistances can be avoided by the correct use of antibiotics. However, this is wrong: the development of resistance is part of bacterial evolution. Resistance can neither be predicted, nor avoided,’ the KIT Congress President explained, adding: ‘in permafrost soil, in bacteria that are more than 30,000 years old, the same resistance genes were found that we see today in vancomycin-resistant enterococci (VRE). It’s true, however, that the spread of resistance genes and of multidrug-resistant organisms (MDROs), does correlate with the use of antibiotics: the higher the use of antibiotics, the faster the development of resistance.’
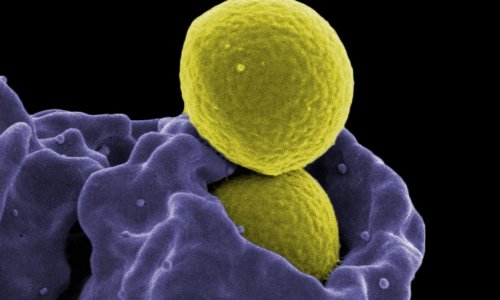
MDROs divide more slowly than sensitive bacteria

Another myth is the claim that MDR bacteria are in general more aggressive than sensitive bacteria. It is correct that MDROs, as a rule, divide more slowly than sensitive bacteria. Resistance genes offer a benefit only when antibiotics are present. If not, they are nothing but a genetic burden. In people who carry MDROs, this reduced biological fitness of the MDROs leads to the human flora being able to overwhelm the MDROs if no antibiotics are administered over a lengthy period of time. ‘Increased mortality in the case of severe MDRO infections is mostly due to the fact that the initially administered antibiotics did not help because, in the early stages of an infection, the physician does not know which type of pathogen caused the infection and thus treats “on suspicion”. Today, detection takes one to two days, which is exactly why we need faster diagnoses,’ Pletz emphasised.
The fact that no new antibiotics are being developed is, above all, an economic issue, since their development can take up to ten years and can cost up to one billion US dollars. To make this investment volume economically feasible, Pletz and colleagues demand an extension of patent protection as in the USA. ‘There is reason to hope, because recent literature describes many substances with antibacterial effects that have the potential for clinical development,’ Pletz said, addressing another widespread misunderstanding.
It is equally misleading to describe MDROs as a mere hospital problem. Whilst, in Germany, MRSA is found mainly in hospitals and numbers are decreasing, other types of pathogens are gaining ground, such as multi-resistant gut bacteria, so-called ESBL-producing bacteria, which enter the body via food. In Germany, 10-13 per cent of patients admitted to a hospital are found to carry this pathogen; in India, 40-60 per cent of the general populace are colonised. They are not eradicated by antibiotic therapy – quite the contrary, further resistances are created.
Either rapid diagnostic tests for biomarkers in the blood, to find out whether we are dealing with a viral or a bacterial infection. Or direct detection of pathogens in a rapid test
Mathias Pletz
The renowned infectiologist proposes a three-pronged approach to fight antibiotic resistance: ‘The alpha and omega is a rational approach to antibiotics in line inter alia with the Antibiotic Stewardship Programme (ABS), which is tested and demanded in hospitals. Another important issue is proper hospital hygiene. It is the only way to effectively prevent MDRO transmission from one patient to another. Last and by no means least, there is vaccination, e.g. influenza and pneumococci vaccinations are effective measures to reduce the number of antibiotics prescriptions in the out-patient sector and thus to reduce the development of resistances.’ Today, quality management of antibiotics prescriptions is well established down to the general hospital level. However, this does not solve the problem in the non-hospital sector where, indeed, 85% of all antibiotic prescriptions are generated, mostly with neither lab results nor X-rays (www.rai-projekt.de).
There are two possibilities to increase the safety of decisions for or against antibiotics: ‘Either rapid diagnostic tests for biomarkers in the blood, to find out whether we are dealing with a viral or a bacterial infection. A study conducted in Hanover showed that, with such a rapid test, we would be able to reduce antibiotic prescriptions by general practitioners (GPs) by up to 60 percent. The second option is the direct detection of pathogens in a rapid test. Last winter we benefited immensely from an influenza rapid test done with a throat sample. This test detects viruses within 20 minutes and we used it right in the emergency room.’ However, as Pletz points out, many of these rapid tests are not reimbursed.
No antiseptics without indication

Another problem, which is almost as pervasive as antibiotic resistances, are hospital-acquired (HA) – called nosocomial – infections. The number of the six most important HA infections is twice the number of the 32 most relevant contagious diseases. Europe-wide, this translates into 2.6 million infections and approximately 90,000 deaths per year.
Infections caused by exogenous pathogens are easier to avoid than those caused by endogenous pathogens. ‘In the past few years research has focused on antiseptics, since they can reduce endogenous bacteria. Since antiseptics don’t kill microorganisms selectively, their use needs to be plausible and it needs to be part of hospital-wide hygiene plans and policies. Non-targeted use does carry certain risks and is to be avoided,’ said Professor Simone Scheithauer, Vice President of the Congress and Head of Central Hospital Hygiene and Infectiology at University Hospital Göttingen, Germany.
The case of the central venous catheter (CVC) illustrates the benefits and limitations of antiseptics. ‘Rather than using a fast alcoholic substance or a mixture of alcohol and PVP iodine to disinfect the entry on the skin, over the past few years a combination of alcohol and octenidine respectively chlorhexidine with remanent efficacy has become popular. In 2015, Mimoz et al. published their results in The Lancet showing that the use of chlorhexidine significantly reduced catheter-induced sepsis,’ Scheithauer explains. The German Commission for Hospital Hygiene and Infection Prevention (KRINKO) thus recommends the use of such combination products.
Antiseptic occlusive dressing
With particularly vulnerable patients, or when high infection rates are recorded, the commission at the Robert Koch Institute recommends antiseptic occlusive dressing for vascular access. ‘When local antiseptic administration is effective it makes sense to apply the substance right at the risk site, usually as impregnated occlusive dressing,’ said Scheithauer. ‘Even with low benchmarks, a significant reduction of venous catheter-associated infections was confirmed.’
Antiseptic wash should be the last resort. This additional measure requires an indication and the pros and cons have to be thoroughly considered. Increasing resistance towards these antiseptics might lead to these substances being ineffective with exactly those patients who would benefit most from them.
Vaccination offers individual and herd protection

Vaccination is meant to achieve different objectives depending on the vaccine: in addition to preventing an infectious disease with possible sequelae for the individual person, vaccination aims to build up herd protection, i.e. the protection of patient groups who cannot be vaccinated. Obviously, another objective is eradication of the pathogen. Vaccination can create a protection between generations. ‘A typical example of herd protection in a family is the vaccination against pneumococci. These pathogens can cause pneumonia and sepsis and are particularly frequent among infants and older people. When infants and children are vaccinated, the serotypes disappear not only in vaccinated people, but also in in the older, non-vaccinated herd,’ said Professor Markus Knuf, Medical Director of the Paediatric Clinic of Dr Horst Schmidt Clinics in Wiesbaden, Germany.
As far as ’flu is concerned, children are the linchpin of transmission. Relatively speaking, they contract influenza more frequently than adults because their immune system has not yet matured and because they haven’t yet had sufficient contact with influenza. Children thus discharge a high number of viruses. Moreover, there are anatomical and behavioural factors that facilitate pathogen spread. If we manage influenza among the youngsters, this might reduce the number of cases in adults. However, there are no really effective vaccines for small children.
On the other hand, adults who are vaccinated can protect children who are too young to be vaccinated from pertussis. Protection has to be renewed every six to eight years. Today, pertussis is seen most frequently among teenagers. It is often misdiagnosed as chronic bronchitis and we increasingly see teenagers infect non-vaccinated infants. In very small children, pertussis is more severe and can be lethal.
Varicella vaccination not only aims to reduce varicella complications but also herpes zoster incidence. Adults can be protected from reactivation by a specific herpes zoster vaccine
Markus Knuf
Varicella, known as chickenpox, is often considered a harmless childhood disease. Indeed, before a vaccine was available, chickenpox mainly affected children. About five per cent of varicella cases are associated with complications, which translates into 35,000 cases alone in Germany per year.
Herpes zoster reactivates varicella and can thus be rightfully considered a sequela. ‘About 50 percent of chickenpox patients also contract shingles. Thus, varicella vaccination not only aims to reduce varicella complications but also herpes zoster incidence. Adults can be protected from reactivation by a specific herpes zoster vaccine. A vaccine, however, that had been available for about ten years turned out to be insufficiently immunogenic,’ Knuf pointed out. ‘A new formula containing an adjuvant promises significantly better results.’
Profiles:
Professor Mathias Pletz MD specialises in internal medicine and pulmonology and is also certified in infectiology and hospital hygiene. He gained his medical degree in Leipzig, Germany, and then became a research fellow at Emory University’s Rollins School of Public Health and at the Centers for Disease Control and Prevention in Atlanta, USA, for two years. In 2008, he received his habilitation and in 2011, he became Professor of Clinical Infectiology at Friedrich Schiller University Jena.
Professor Simone Scheithauer MD graduated in 2000. Seven years later she became a consultant in medical microbiology, virology and infectious disease epidemiology. She was appointed consultant for hygiene and environmental medicine in 2010 and, in 2012, became a consultant for infectious disease. From 2014 she has headed the division for infection control and infectious diseases at the University Hospital Göttingen, where she became a professor in 2015. Very recently a professorship has also been offered in Göttingen, Germany.
Having studied medicine in Münster and Mainz, Professor Markus Knuf MD, in 1997 completed his 5-year training as paediatrician at University Hospital Mainz, with a focus on infectiology, paediatric immunology and neuropaediatrics. From 2001-09 he was a consultant at the Mainz centre; he then became director of the paediatric clinic in Wiesbaden and was appointed chair of paediatric infectiology and interdisciplinary paediatric intensive medicine at the University of Mainz.
14.04.2019