Article • Resistance-building
‘Why not take a risk?’ belief boosts antibiotic overuse
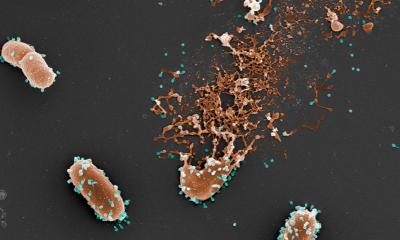
Antibiotics are mostly prescribed for acute respiratory infections (ARIs), yet most of these infections are viral. A new study shows that inappropriate antibiotics prescriptions are widespread, contributing dangerously helping antibiotic-resistant organisms to grow.
Source: Shutterstock/mathagraphics
Overuse could be due to attitudes among patients and clinicians, current George Washington University research suggests. Understanding prescribing practices is important which is why a group of scientists led by Fiona P. Havers, MD, from the Centers for Disease Control and Prevention in Atlanta, Georgia, USA, designed a study to analyse out-patient antibiotic prescribing for ARIs during influenza seasons and to find targets to improve antibiotic stewardship.
The cohort study enrolled outpatients aged six months or older with ARI evaluated at out-patient clinics associated with fi US Influenza Vaccine Effectiveness Network sites during 2013-2014 and 2014-2015 influenza seasons. All patients had influenza tests. Antibiotic prescriptions, medical history, and diagnosis codes were collected from medical and pharmacy records, as were group A streptococcal (GAS) testing results in a patient subset.
The researchers found that antibiotics were likely prescribed inappropriately to a great number of the 14,987 out-patients in the study who presented with symptoms of a broadly defined ARI characterised by cough. Among all those prescribed antibiotics, 41% lacked a diagnosis code for which antibiotic therapy is potentially indicated. Most suffered viral upper respiratory tract infections and bronchitis. Those with influenza confirmed through research testing accounted for a substantial proportion (17%) of all antibiotics prescribed, yet fewer than a third of laboratory-confirmed influenza patients were given a clinical diagnosis of influenza.
The results strengthen the call for improved antibiotic stewardship. Increased efforts are needed to support adherence to prescription guidelines and improved point-of-care influenza diagnostics and recognition. Increased access to sensitive and timely virus diagnostic tests, particularly for influenza, could reduce unnecessary use. However, the USA’s George Washington University research suggests there is another rooted problem in over prescription: a ‘Why not take a risk?’ mentality is widespread among patients and care providers.
Improve communication
Unfortunately, this individually rational action leads to negative consequences for society
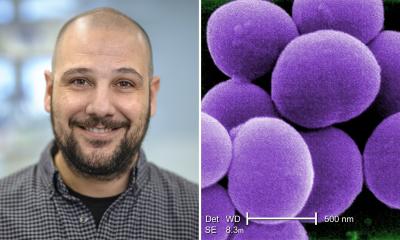
David Broniatowski
Led by David Broniatowski, assistant professor in George Washington University’s engineering management and systems engineering department, the study analysed patients’ and cAnlinicians’ perceptions of antibiotic prescribing for upper respiratory infections in acute care. They surveyed clinicians and patients from two large urban academic hospital emergency departments (EDs) and a sample of nonpatient subjects regarding their bottom-line understanding of information about antibiotics according to fuzzy trace theory, as well as relevant knowledge and expectations.
While clinicians demonstrated greater knowledge of antibiotics and concern about side effects than patients, the predominant categorical gist for patients and clinicians was ‘why not take a risk,’ which compares the status quo of remaining sick to the possibility of benefit from antibiotics. Many knew antibiotics do not work against viruses, yet the providers still believed the antibiotics might help patients feel better. Side effects from antibiotics were often thought essentially nil for the individual patient, Broniatowski said. ‘Unfortunately, this individually rational action leads to negative consequences for society.’
Thus communication strategies directed at patients and providers are needed, along with sensitive testing and guideline adherence, to reduce inappropriate prescribing.
19.07.2018