Source: Boris Brkljačić
Article • Multiparametric ultrasound
Experts assess usefulness of MPUS in the diagnostic conundrum
Multiparametric ultrasound (MPUS) has proven its value in the abdomen – now, the technique is increasingly moving towards peripheral areas such as breast and testis imaging, experts showed in a dedicated session at ECR 2022.
Report: Mélisande Rouger
Breast imaging
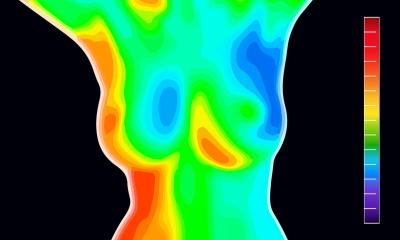
MPUS has been used in breast imaging for many years and the most commonly used features are black-and-white, grayscale and B-mode, Professor Boris Brkljačić, Professor of Radiology and Vice-Dean at University of Zagreb School of Medicine in Croatia, told the audience. ‘The majority of our diagnosis and criteria to differentiate benign and malignant lesions are based on B-mode ultrasound,’ he said.
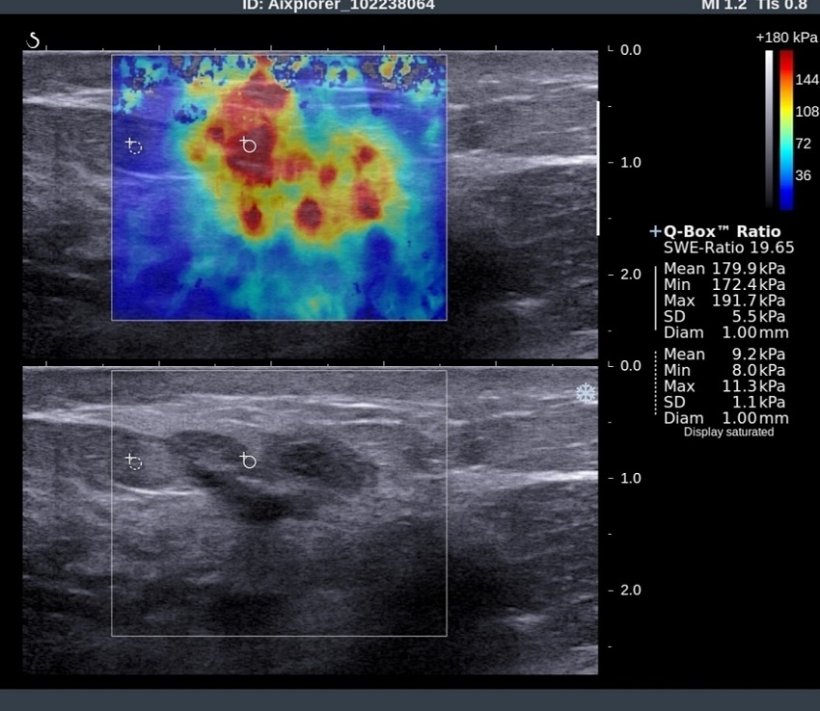
Brkljačić routinely uses colour Doppler to assess vascularization of lesions. And in the last 15 years, he has been using elastography to assess lesion elasticity and stiffness. ‘Most cancers are stiff, while most benign lesions like adenoma are soft,’ he said. ‘This difference can be evaluated and quantified with elastography.’
Contrast-enhanced ultrasound (CEUS) in the breast is mostly used for research purposes, but it could help assess treatment response to neoadjuvant therapy in breast cancer that can be treated with chemotherapy and surgery, Brkljačić explained. ‘The success of chemotherapy can also be evaluated with contrast-enhanced MRI, which is the standard procedure used for this purpose, but CEUS might have a role to play here, especially since it’s far more available than MRI,’ he said.
Ultrasound requires a lot of experience and the ability to work with modern equipment that offers software support for special features in B-mode and elastography. ‘In B-mode, for example, it’s important to use compound and harmonic imaging,’ he explained.
Ultrasound can also help guide biopsy or prepare for surgery. ‘If you see a lesion on mammography and MRI, it’s very easy to perform ultrasound-guided biopsy and deposit clips under ultrasound guidance before neoadjuvant therapy,’ he said. ‘You can also puncture lymph nodes in the axilla using ultrasound guidance, as it’s much easier and faster than under mammography or MRI guidance.’ Ultrasound-guided biopsy enables to make a very reliable diagnosis in the preoperative stage, with all the necessary information on oestrogen receptors, progesterone receptors, HER2 status, proliferation, etc.
Mammography remains the first modality for breast cancer primary diagnosis and screening. However, the European Society of Breast Imaging (EUSOBI) recommends that women with very dense breasts should be examined with abbreviated MRI protocols. But when MRI is not available, radiologists should not hesitate to rely on ultrasound. ‘In dense breasts, accuracy of mammography is lower. An additional test with ultrasound can help detect breast cancer. MRI is better, but we don’t have the possibility to screen every woman with MRI, so ultrasound is a good alternative.’

Testis imaging
In the testis, the challenge for MPUS remains to characterize lesions, according to Michele Bertolotto, Associate Professor of Radiology at Trieste University in Italy, who also spoke in the session. ‘When you find a small, non-palpable lesion in the testis, although you’re able to identify it with very high sensitivity, typically you’re not able to characterize it,’ he said. ‘All lesions, either benign or malignant, look similar on ultrasound.’ There is a necessity to improve characterization of such lesions to avoid unnecessary surgery, he argued. ‘70% of these lesions are benign or non-neoplastic,’ he said. ‘If you perform orchiectomy each time, there’s a lot of over-treatment.’
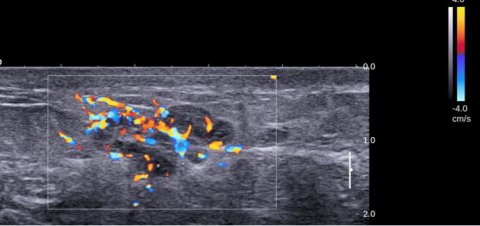
Urologists still recommend removing the testis when lesions are not characterized well enough, as a risk of cancer remains. ‘It’s crazy, many patients still undergo surgery for benign lesions,’ Bertolotto insisted. But even urologists begin to understand that this is an issue, as the literature increasingly shows the benefits of following up lesions over time, he added. Specificity can often be improved, and CEUS allows to assess with very high specificity whether the lesion is vascularized or not. ‘In practice, all the lesions that are avascular on CEUS are benign or non-neoplastic,’ he explained. ‘If lesions are vascularized, it’s more complicated. Still, you can follow up or only remove the nodule, not the whole testis.’
Elastography and Doppler can be useful in that setting. If the lesion remains stable with these parameters, follow up should continue. If vascularization or consistency on elastography increases, it is an indication that the lesion could be malignant.
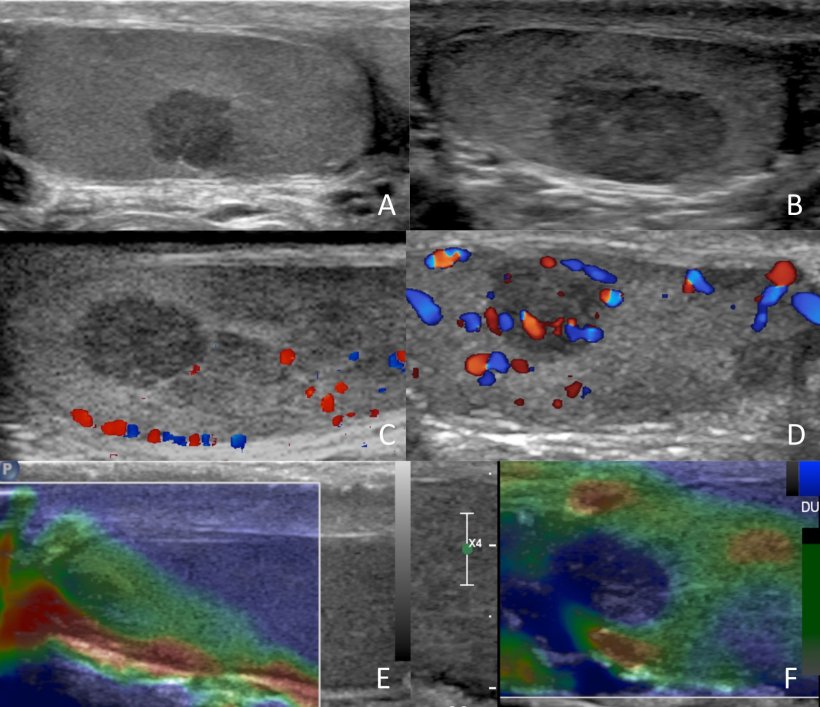
Image source: Prof Bertolotto
Ultrasound is a multistep examination, Bertolotto reminded the audience. ‘Incidental findings typically occur when a patient undergoes an ultrasound scan for infertility or because he has some pain or discomfort.’
The next step is to carry out a colour Doppler test, to see if the lesion is vascularized or not, what its consistency is on elastography, and then to complete this test with CEUS. ‘If you have a soft lesion that becomes harder in time, it’s a sign of malignancy. Any change is a sign of potential malignancy,’ he said.
If lesions are not palpable and do not show a suspicious behaviour during follow-up, Bertolotto strongly recommends not undergoing surgery. ‘Most patients who present with infertility are young. You would reduce their possibilities to conceive if you remove a testis,’ he concluded.
Profiles:
Boris Brkljačić is Vice-Dean for International Cooperation, Full Professor of Radiology and Chair of Radiology Cathedra, University of Zagreb School of Medicine, Zagreb, Croatia. He is also the immediate past-president of the European Society of Radiology, and the General Secretary of the International Society of Radiology and the president of EURAMED.
Michele Bertolotto is ESUR President-elect, senior consultant in genitourinary radiology, and chief of ultrasound at the department of Radiology of the University of Trieste, Italy.
13.07.2022