Article • Interdisciplinary senology
Mammography, ultrasound, MRI: which imaging modality at which time?
Interdisciplinary collaboration between gynaecologists, radiologists, pathologists and breast care nurses following a palpation finding makes a decisive contribution to the success of further breast cancer treatment. This was the consensus among the speakers at the Annual Congress of the German Society of Senology in Dresden. The experts provided clear explanations of which imaging is best for which patient.
Article: Sonja Buske
© Cipta – stock.adobe.com
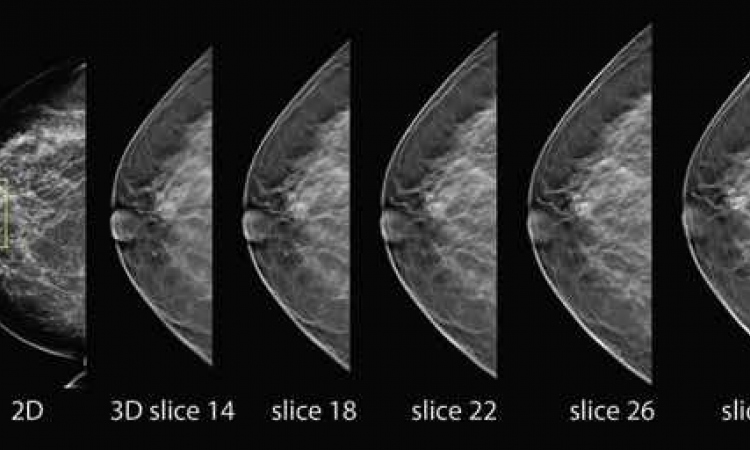
PD Dr Susanne Wienbeck, a specialist in radiology at St. Josef-Stift Bremen, made it clear that both mammography and sonography are first choice methods for clarifying the next steps after an initial palpation finding. Which of the imaging procedures should be used depends largely on age: ‘Patients under 40 should always have a clinical ultrasound scan first,’ emphasised Wienbeck. ‘If the result is clearly benign, for example a cyst or fibroadenoma, no further clarification is necessary,’ she continued. ‘In the case of suspicious or unclear findings with a low risk, a sonographic punch biopsy should be performed. Advanced imaging such as mammography, followed by an open or percutaneous biopsy, is only recommended for high-risk findings.’
Current studies further show that preoperative MRI reduces the number of resections in breast-conserving surgery
Heike Preibsch
Things are different however for patients over the age of 40. Here, the radiologist is in favour of mammography as a first step, followed by extended imaging if there are multiple or unclear findings. In addition to the palpation diagnosis, suspicious skin changes, histologically confirmed lesions or unilateral mastodynia are also indications for a mammogram, she added.
Pre-operative MRI has long been suspected of increasing mastectomy rates. ‘However, this has been proven not to be the case,’ emphasises PD Dr Heike Preibsch, Senior Physician at the University Hospital of Tübingen. ‘Current studies further show that preoperative MRI reduces the number of resections in breast-conserving surgery.’ The expert went on to explain that not only patients with dense breasts would benefit from this, but that the advantage applies across all entities, stages and risk constellations. ‘Our ultimate goal should always be primary R0 resection.’
Clear communication of findings between all disciplines
Dr Anna Marie Maier from the Clinic and Polyclinic for Gynaecology and Obstetrics at LMU Klinikum Munich sensitised the audience to the importance of comprehensive communication of findings. ‘Discussing further diagnostics and the intended markings is essential, as is intraoperative assessment. All professional groups involved should be included in order to be able to describe their point of view,’ said Maier. Further, presentation to the tumour board is also absolutely essential, both pre- and post-operatively.
01.09.2024