News • Neuropilin-1 as a 'helper' for COVID-19
Coronavirus: Study finds further 'door opener' into the cell
The coronavirus SARS-CoV-2 is known to infect cells via the receptor ACE2. An international research team under German-Finnish coordination has now identified neuropilin-1 as a factor that can facilitate SARS-CoV-2 entry into the cells’ interior.
Image source: DZNE/Liliana Pedro-Domingues
Neuropilin-1 is localized in the respiratory and olfactory epithelia, which could be a strategically important localization to contribute to SARS-CoV-2 infectivity and spreading. Experts from the German Center for Neurodegenerative Diseases (DZNE), Technical University of Munich, University Medical Center Göttingen, University of Helsinki and other research institutions now published their findings in the journal “Science”.
The starting point of our study was the question why SARS-CoV and SARS-CoV-2 that both use ACE2 as a receptor cause different diseases
Mikael Simons
The coronavirus SARS-CoV-2 can affect various organs such as the lung and kidneys and also trigger neurological symptoms, including a temporary loss of smell and taste. The spectrum of symptoms of the associated disease - known as COVID-19 - is therefore quite complex. A related virus, SARS-CoV, led to a much smaller outbreak in 2003, possibly because the infection was limited to the lower respiratory system, making the virus less transmissible. SARS-CoV-2, in contrast, additionally infects the upper respiratory system including the nasal mucosa and, in consequence, spreads rapidly through active viral shedding, e.g. when sneezing.
Tissue tropism reflects the ability of a virus to infect specific cell types in different organs. It is determined by the availability of docking sites, so-called receptors, on the surface of cells. These allow docking to and penetration into the cells. “The starting point of our study was the question why SARS-CoV and SARS-CoV-2 that both use ACE2 as a receptor cause different diseases,” explained Mikael Simons, a research group leader at the DZNE’s Munich site and professor of molecular neurobiology at the Technical University of Munich, whose team was involved in the current studies, together with Giuseppe Balistreri’s group at the University of Helsinki.
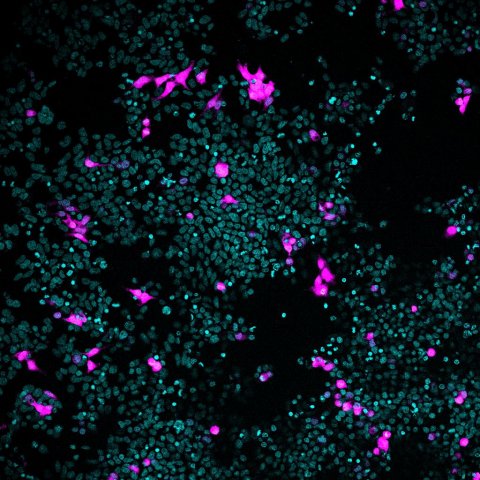
Image source: DZNE/Liliana Pedro-Domingues
To understand how these differences in tissue tropisms can be explained, the researchers took a look at the viral “spike proteins” that are essential for virus entry. “The SARS-CoV-2 spike protein differs from its older relative by the insertion of a furin cleavage site,” explained Simons. “Similar sequences are found in the spike proteins of many other highly pathogenic human viruses. When we realized that this furin cleavage site is present in the SARS-CoV-2 spike protein, we thought that this might lead us to the answer."When proteins are cleaved by furin, a specific amino acid sequence becomes exposed at its cleaved end. Such furin cleaved substrates have a characteristic pattern that are known to bind to neuropilins at the cell surface.
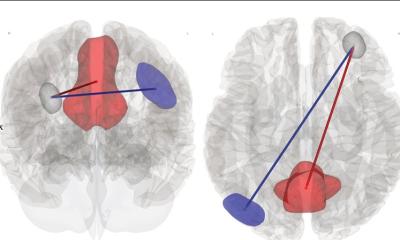
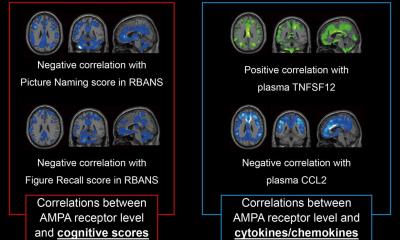
Experiments using cells cultured in the laboratory, in conjunction with artificial viruses that mimick SARS-CoV-2 as well as naturally occurring virus, indicate that neuropilin-1 is able to promote infection in the presence of ACE2. By specifically blocking neuropilin-1 with antibodies, infection was suppressed. “If you think of ACE2 as a door to enter the cell, then neuropilin-1 could be a factor that directs the virus to the door. ACE2 is expressed at very low levels in most cells. Thus, it is not easy for the virus to find doors to enter. Other factors such as neuropilin-1 might be necessary to help the virus,” explained Simons.
Recommended article

News • Coronavirus disease symptom
Exploring why COVID-19 makes people lose their sense of smell
Doctors have reported that partial or total loss of the sense of smell is often an early symptom of infection with SARS-CoV-2, the virus that causes COVID-19. Now, researchers reporting in ACS Chemical Neuroscience have shown that in mice, two proteins required for SARS-CoV-2 entry are produced by cells of the nasal cavity that contribute to odor detection.
Since loss of smell is among the COVID-19 symptoms and neuropilin-1 is mainly found in the cell layer of the nasal cavity, the scientists examined tissue samples from deceased patients. “We wanted to find out whether cells equipped with neuropilin-1 are really infected by SARS-CoV-2, and found that this was the case,” said Simons. Additional experiments in mice showed that neuropilin-1 enables transport of tiny, virus-sized particles from the nasal mucosa to the central nervous system. These nanoparticles were chemically engineered to bind to neuropilin-1. When the nanoparticles were administered to the nose of the animals, they reached neurons and capillary vessels of the brain within few hours — in contrast to control particles without affinity for neuropilin-1. “We could determine that neuropilin-1, at least under the conditions of our experiments, promotes transport into the brain, but we cannot make any conclusion on whether this is also true for SARS-CoV-2. It is very likely that this pathway is suppressed by the immune system in most patients,” explained Simons.
“SARS-CoV-2 requires the ACE2 receptor to enter the cells, but other factors such as neuropilin-1 may be required to support its function,” said Simons. “However, at present we can only speculate about the molecular processes involved. Presumably, neuropilin-1 catches the virus and directs it to ACE2. Further investigations are needed to clarify this issue. It is currently too early to speculate whether blocking neuropilin could be a viable therapeutic approach. This will have to be addressed in future studies.”
Source: German Center for Neurodegenerative Diseases (DZNE)
21.10.2020