Article • Screening
Can, should and must MRI replace mammography?
In breast cancer care each patient receives personalised, highly effective diagnosis and treatment procedures. In breast diagnostics this mainly revolves around new MRI scanning procedures that allow the quantification of biological and physiological processes on a cellular and molecular level.
Report: Daniela Zimmermann

'The talk here is of molecular MRI (mMRI), which even today makes it possible to differentiate between benign and malignant breast cancers without needing biopsies, with an impact on treatment procedures – such as minimising over-diagnosis – and of the early prediction of the therapy response of individual cancers,’ says Professor Thomas H Helbich, Vice Chairman of the University Department of Radiology and Nuclear Medicine at Vienna’s Medical University.
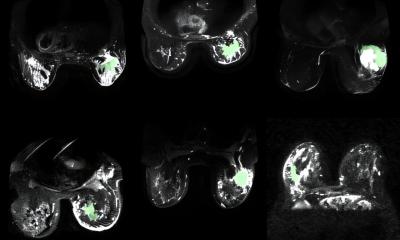
During this year’s MR symposium in Garmisch, his lecture centred on mMRI. Various processes, such as tumour angiogenesis, cell proliferation, molecular movement and numerous metabolic changes, play a key role in the development of breast cancer. mMRI facilitates the quantification of these key processes on a cellular and subcellular level. ‘The combined use of different MRI procedures, such as contrast enhanced MRI, diffusion weighted imaging (DWI) and MR-Spectroscopy (MRS) provides first insights into the world of mMRI. This method allows us to measure multiple imaging biomarkers simultaneously and non-invasively,’ Prof. Helbich explained. It has been shown that the acquisition of these parameters enhances specificity considerably without overlooking breast cancer. Therefore he advocates increased use of mMRI in routine breast diagnostics.
MRI also plays a vital role in monitoring cancer therapy. Depending on the chosen procedure it enables doctors to differentiate between cancers that do or do not respond to treatment shortly after it begins. This means, the professor explains, that MRI meets all the requirements for implementation in personalised medicine: Treatments that do not have the right effect can be replaced by more efficient procedures.
The enhancement of mMRI through PET constitutes a further quantum leap for the implementation of personalised medicine. Fluorodeoxyglucose (18F-FDG) PET measures the glucose metabolism, which increases in tumour tissue compared to normal cells. Additionally, PET allows precise imaging using specific radiotracers. These can capture different, relevant processes of tumour development, progression and therapy response, such as tumour hypoxia, apoptosis, cell proliferation or receptor density. ‘In a recent study, our Working Group showed that PET-MRI facilitates improved, non-invasive differentiation of benign and malignant breast cancers. The procedure can achieve a reduction in the rate of unnecessary biopsies by 50%,’ the professor confirmed.
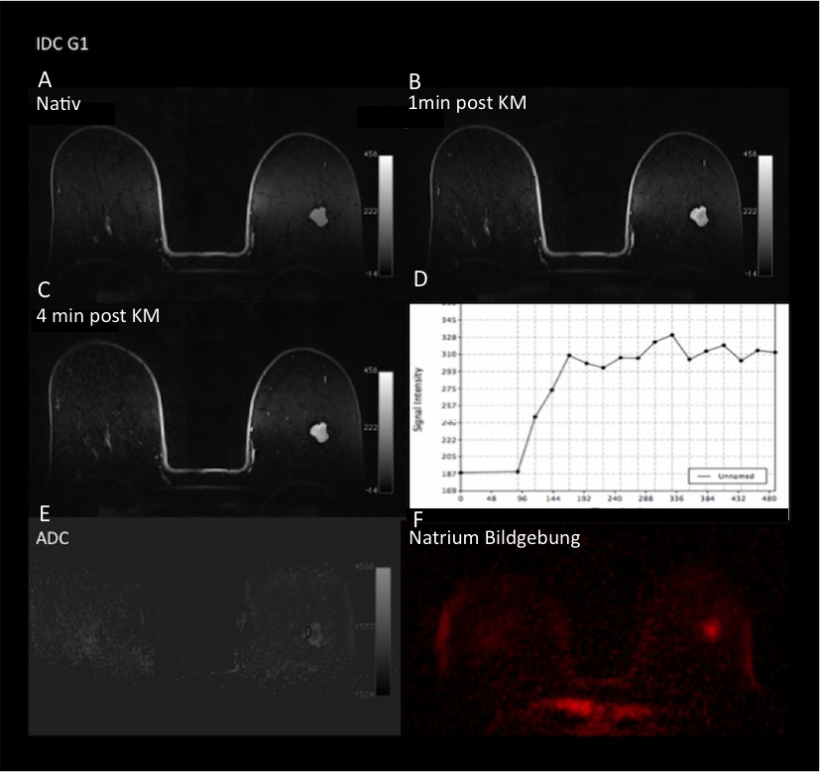
increased concentration of sodium. mMRI shows that the lesion is without doubt a malignant one (BI-RADS 5).
Despite all its advantages, breast-MRI, which resulted from pioneering work by two German radiologists i.e. Professors Sylvia Heywang Köbrunner and Werner Kaiser – who unfortunately passed away far too early – currently doesn’t fare too well in its ‘homeland’, a development that Prof. Helbich views critically. Undoubtedly, breast MRI has not become a routine examination but should be carried out when and where indicated. However, the wide range of indications for breast MRI should not be limited by an evidence-based view of medicine with a limited focus. ‘Breast MRI is of benefit for pre-operative staging, such as for invasive lobular cancers and for non-invasive ductal cancers. It is also successfully being utilised for neo-adjuvant chemotherapy and is undisputedly the best method to differentiate between scar tissue and recurrence. Furthermore, it is also the best procedure for high risk screening,’ he added: ‘In particular, the data for high risk screening with MRI show that a large proportion of clinically significant breast cancers are detected far too late with mammography and ultrasound compared to MRI scanning. Therefore it’s no surprise that some countries are already considering considerably shortening the MRI protocols for breast imaging and establishing MRI for screening in place of mammography.’
Profile:
Dr Thomas H Helbich MSc MNA is a professor and Vice Chairman of the University Department of Radiology and Nuclear Medicine at the Medical University of Vienna. As an expert in breast cancer diagnosis he was previously in charge of the Breast Imaging Department at the University of Toronto.He is also a past-president of the European Society of Breast Imaging (EUSOBI) and the Austrian Society of Senology (ÖGS) (2009-2011).
06.03.2015