Article • Mammo update
Breast cancer: Why MRI should not be a political decision
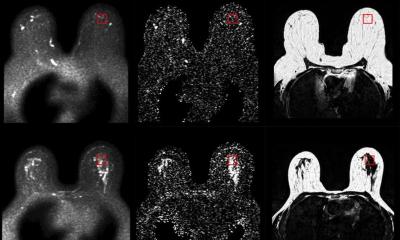
A paper of Professor Christiane K Kuhl and her colleagues had discovered that, to detect pre-invasive breast cancer (DCIS), the addition of high-resolution MRI and state-of-the-art mammography offered a significantly higher sensitivity compared with state-of-the-art mammography.

When we asked Prof. Kuhl why the University of Bonn was cited by her Discussant at ASCO to carry out the most breast MRI examinations in, perhaps, the entire world, she said it was possibly true, explaining: ‘We have a very good team here and we have reserved one MR system more or less for breast examinations. Bonn also has a large, supra-regional catchment area. Many women - some who might have a known risk of breast cancer in the family - come to us of their own accord – for example, if they have had MRI examinations elsewhere and the results are not clear.
‘I’m often asked what radiologists should do to achieve results on a par with those we have in Bonn. The answer is quite simple: Radiologists should carry out more breast MRIs. Unfortunately this procedures is not utilised enough as the medical insurers quite often refuse to cover it, because they say it’s too expensive! Magnetic resonance tomography did not arrive yesterday. It is an examination procedure that many areas of modern medicine can no longer do without. Think about orthopaedics or neurosurgery, for instance. MRI is of great importance in those fields. It has also been known for some time that MRI is the most sensitive examination procedure for the diagnosis of invasive breast cancer.
'With MRI you play in an entirely different league compared with conventional mammography or ultrasound. This has been known for years. However, as the procedure is expensive, so far MRI has mainly been used in a “targeted” way, i.e. when a patient has already suffered breast cancer and then later receives results from an X-ray mammography or ultrasound scan that are not quite clear. Then, and only, then, is the breast MRI covered by Germany’s statuary medical insurers - apart from a few other, still rare indications.
The chronic under-usage of this examination procedure [MRI] is therefore both the result and the cause of the current situation
Christiane Kuhl
‘However, the medically meaningful, or possibly even more important, potential areas of use, such as pre-operative staging or early detection are not covered. Staging means that if a type of breast cancer is detected by mammography or ultrasound, which is to be treated by breast conserving surgery (bearing in mind that over 80% of women are treated with breast-preserving procedures) then an MRI should be carried out prior to the operation to map the actual spread of the tumour. This use of breast MRI – staging – is not yet covered by medical insurers in Germany as standard, which I consider scandalous.
‘The consistent use of MRI prior to surgery for breast cancer would have a significant impact on the treatment management for around 25% of patients. Breast cancer is a type of oncological disease where the surgical approach is curative, which is quite rare in oncology. And, of all things, it is just this situation where MRI cannot be used. However, it is used regularly in almost all other areas of oncology, such as, for instance, in patients with pancreatic carcinoma, which are rarely approached in a curative manner. This is a contradiction!’
Why? ‘Cost is one factor. Breast cancer occurs much more often than pancreatic cancer. Secondly, the breast MRI only helps us in this situation when we can verify the MR diagnoses histologically for the surgeon and mark the area for surgery. Radiologists have quickly internalised and started to use the biopsy procedure for X-ray mammography, or ultrasound, and also the vacuum biopsy. But people still seem to shy from MRI-controlled biopsies – although they are no more complex than mammotome biopsies (particularly with the modern VAB systems, such as the Suros system). The problem again is that MRI can be used only infrequently, which essentially makes systems for MR guided procedures less profitable. The chronic under-usage of this examination procedure is therefore both the result and the cause of the current situation. Medical insurers don’t pay for it because the procedure allegedly produces too many wrong, positive results, therefore radiologists cannot use it – and then, if the procedure is actually used once in a while, results are insufficient and nobody is able to confirm these additional results adequately and in a minimally-invasive manner, which, quite rightly, leads to irritation and uncertainty among surgeons. In turn, this damages the reputation of this procedure and strengthens the insurers’ perception that it is expensive and unsuitable – which is why it is not covered. That’s how the cycle closes – and has done for years.
‘There is a further issue: Radiologists specialising in breast examinations use mammography and ultrasound almost exclusively and therefore have great expertise in this area - they specialised in this at a very early stage. They have few or no points of contact with MRI. To them, MRI is like an “exotic animal”. This unsettles them. Whenever I say: “MRI should be carried out as standard as part of any breast-preserving therapy,” all I hear from the mammographers is “But who is going to pay for this?” And this is despite the fact that we are looking at one of the - if not the most extensively researched area of application for MRI in terms of clinical relevance. If these mammographers were to spend just one day in an MRI department they would be amazed at what is being examined with MRI these days, without “costs” being raised – for example, MRI of the spinal lumbar region, for which we know there is little clinical relevance and which has little impact on therapy management for these patients.’
This is changing increasingly in the USA, she pointed out, there breast MRI is seeing enormous growth rates. Guidelines from the American Cancer Society stipulate that all women with a lifetime-risk of only 20% are to receive a breast MRI for early detection. ‘This goes even further than the data currently available would call for,’ said Prof. Kuhl. ‘These data, a not insignificant proportion of which was collected in Bonn, state that women who are at higher risk due to the disease having familial history, should receive an annual MRI for early detection. And a risk of 20% is reached quite quickly.
‘In future, all those women in the US will be examined with MRI for early detection. But, in Germany, MRI for early detection is not being considered, even though this procedure is more or less a German product, and despite the fact that the data on which the recommendations are based originated mainly here and Europe. At the same time we know from new data from the DMIST study, carried out by Etta D Pisano, that the medium sensitivity of mammography is between 40-50%, i.e. out of 10 women suffering from breast cancer only 4 or 5 are actually detected, the rest are sent home as healthy, because mammography cannot visualise these cancers.
‘For women who are at average risk, we don’t know what the comparative sensitivity rate with screening MRI is, as yet. But the sensitivity of MRI for screening women at increased familial risk has been twice as high or, in some cases, more, up to three times as high as mammography, in all published studies. Breast MRI has a sensitivity of over 90%, mammography of 33-40%, combined with ultrasound this increases to 45-50%. By the way, this corresponds with data from the DMIST study - the only mammography study that has actually validated its data. Since our first publication in 2000, over 10,000 women have been examined, and more studies have been published in high-quality journals (NEJM, JAMA, The Lancet etc.). The results are surprisingly concordant: MRI is far more efficient than mammography and ultrasound — also for women who are only at moderate risk of developing breast cancer.
G3 invasive carcinoma are very dangerous indeed. Therefore, it’s essential to detect them at the in-situ stage – once they grow invasively, the race is on
Christiane Kuhl
Asked whether these convictions could mean the end for an entire industry, Prof. Kuhl replied: ‘I wouldn’t put it quite that way! Mammography definitely has its place, and we should also not say we want to carry out only MRI. But what we want to be able to do is to also carry out MRI. It cannot be right that, in 2007, a mammography screening project in Germany - for many millions - is based on technology delivering this level of sensitivity – using technology with well-known limitations. About 40 years ago, when screening projects began in Scandinavia, there was no other technology available. Today, we know all the mammography figures, they are on the table. Mammography cannot visualise many carcinomas - due to limitations inherent in this procedure, not bad technology or because a radiologist lacks training. Even with the best technology and highest radiological expertise, certain carcinomas cannot be detected for purely physical reasons, because they are embedded in dense glandular tissue. We have known for some time that ultrasound can counterbalance some of mammography’s shortcomings, but we should assume that MRI can do this even better. Therefore we must invest in this procedure – in order to make it ready for use in screening.
‘We have known for quite a while that MRI, compared with mammography and ultrasound, is better for diagnosis of invasive breast cancer. However, people have said for years that MRI cannot visualise pre-breast cancer stages - intraductal carcinoma or ductal carcinoma in-situ (DCIS). It was thought this was the sole domain of mammography. To explain this in more detail: Most breast cancers – 80-90% - develop in cells that build the inner lining of the milk ducts. There is a phase in almost all cancers where real tumour cells are already present, but where they remain in the milk ducts for a certain period of time. Therefore the term ductal carcinoma in-situ is used.
‘At this point we are formally talking about cancer cells. Biologically though, for the patient the situation is still benign, because the cells are surrounded by the walls of the milk ducts and have no connection to blood or lymph vessels. At this stage breast cancer is therefore always curable.
‘If you find breast cancer at this in-situ stage this can be considered the “Holy Grail” of early detection. Prior to mammography, DCIS was not diagnosed prospectively, but was virtually always an incidental finding made at pathology. Since the introduction of mammography, around a fifth, i.e. 20% of carcinomas at the in-situ stage have been diagnosed, which is a reason why early detection with mammography works. As microcalcifications cannot be visualised via ultrasound or MRI, it was assumed that the diagnosis of in-situ carcinoma is possible only with mammography. In fact, in-situ carcinoma can be visualised very well with MRI, they just look different to invasive carcinoma.
‘We know that in-situ carcinoma can be divided into two categories: High-grade and non-high-grade. Non-high-grade means that carcinomas are dormant for years and possibly never turn invasive. Of the high-grade ones we know essentially that they always become invasive and that the intraductal phase is very short. The high-grade, i.e. G3 invasive carcinoma are very dangerous indeed. Therefore, it’s essential to detect them at the in-situ stage – once they grow invasively, the race is on.
‘The interesting feature of our data is that, very unexpectedly, MRI has proved not only on a level with mammography in the detection of in-situ carcinomas but, in fact, significantly superior – particularly in the diagnosis of high-grade in-situ carcinoma. In the detection of 167 in-situ carcinomas the sensitivity of mammography was 51%, MRI was 92% - figures that are clearly in favour of MRI. Mammography was particularly insufficient to diagnose high-grade in-situ carcinomas: it could not detect over half of the high-grade DCIS – because they had not developed any calcifications!
‘It appears that a relevantly high proportion of the in-situ carcinoma does not calcify, so mammography cannot detect it. I said earlier that 20% of all diagnosed carcinoma are in-situ carcinomas. But we know that almost all carcinomas go through this stage – so what happens with the rest? We must assume that MRI will enable us to detect more carcinomas at this early stage, particularly the high-grade carcinoma.
‘Basically, unlike what was previously believed, MRI is superior to mammography also for the pre-invasive stages, the in-situ carcinoma. For the non high-grade in-situ carcinoma both procedures are complementary. For the high-grade in-situ carcinoma they are not complementary – MRI is clearly superior.
‘One of my favourite assumptions (but which cannot be proved) is that the perhaps 10% of DCIS that cannot be detected by MRI are not biologically relevant – because they are not preparing to invade and might never become invasive. For invasive growth, the DCIS requires vessels that deliver nutrients and oxygen. When those vessels are present MRI can detect the DCIS, so quite possibly we can see all those carcinomas that are preparing to invade. If we want to detect breast cancer at an early stage then, quite clearly, we want to detect it at the in-situ and early invasive stages. And we certainly want to find the high-grade carcinomas. If we know that the examination we currently use for early detection - mammography - can only find half of the invasive and intra-ductal carcinomas, then the logical consequence is obvious.
‘Logically, the next question would be whether we will use MRI for screening. Currently we cannot do this, because we still have to gather more data, because we must define exam standards and must establish a quality assurance analogue like that used in mammography, along with training radiologists etc. And even if all this will be settled - using MRI for screening will be expensive. Whether or not we, as a society, want to make this investment is a political, not a medical question.
Dieser Artikel ist auch auf Deutsch vorhanden, bitte klicken Sie hier.
17.07.2009