Breast cancers vary in complexity
Which diagnostic tools work best for which?
Dr Giorgio Rizzatto, who heads the Department of Diagnostic Imaging at ASS 2 Isontina (including the Gorizia and Monfalcone hospitals) in NE Italy, works with nine radiologists, who examine and report on 80,000 clinical and screening breast examinations annually.

In 2000 this department was the second in Italy to adopt full-field digital mammography with a GE Healthcare unit. Today, most of the mobile screening services in Italy are moving from analogue to digital mammography, ‘very very quickly’ Dr Rizzatto told Meike Lerner of European Hospital. There’s just one problem in this transition, he added, when they are mixed together. ‘For ultrasound, we use two GE units, one Esaote unit and we have also a Hitachi unit with elastography, which we use routinely. Almost all patients with nodules, or something suspicious, have elastography. We are very satisfied with its results’ ‘We use magnetic resonance in Italy, but according specific guidelines. In the last five years we had some Italian multi-centre studies of high risk patients and a comparison of mammography, magnetic resonance, and ultrasound. They were published on the major journals . In 2007 we also had a consensus conference in Florence, and the results were published very recently in our journal La Radiologia Medica, both in Italian and in English. The final statement about the use of MR in breast is that in many areas the topic is still under debate. From all the results, MRI seems very good especially for pre-operative staging. But for screening it must be applied only to high-risk patients at the moment. We do not have enough resources and it’s expensive and gives many false positive results, with a lack of specificity. So you have to perform many second look ultrasound examinations to try to pick up the lesions seen with MRI. The other problem is that not all the instruments are good enough for breast MRI. For example if you have spectroscopy you can reduce the number of false positives by looking at the choline peak. So, that’s one major problem. Also, a biopsy costs a lot and is time consuming, and it’s difficult to have the instrument free. Today, my department has scheduled ten breast MRI examinations per week and it is a lot if you consider that usually the Italian centres perform no more than five examinations. That’s the problem.
‘The gold standard is still mammography, and we always start with that. But, with very young patients -- under aged 30 -- we begin with ultrasound, but if we see the breast tissue has a good percentage of fat, we immediately perform a mammogram because mammography is the starting point -- no doubt.
Ultrasound
First, when you have a breast which is very dense on a mammogram, you must search the whole breast for cancers and pathology with ultrasound. That’s the major reason why use ultrasound, other than for palpable nodules, opacities seen on mammography, traumas and infections. Anyway in some cases we have many problems using both mammography and ultrasound. This is the case, for example, in lobular carcinoma. This grows in two different types: nodular, so you have an opacity or a nodule on the mammogram, and that is not so difficult to understand; but in about 40% of other cases lobular carcinoma grows in the so-called Indian line arrangement, meaning lines of tumour cells, surrounded by lines of cells that are normal. In this case, there is usually a nodule or a hard area on palpation, but you see nothing on the mammogram. The echopattern might be often normal also on ultrasound, so you must go inside with a large needle, or you can use elastography, for example, which usually shows the tumoural area quite well.
In other cases, opacity with mammography shows very clear margins, without irregularities or spiculation, and in these you perform ultrasound and you see that the tissue is solid and there’s a lot of vascularity inside, as in some small medullary carcinomas, colloidocysti or mucinous carcinomas, which are not common, but represent at least 5% of cases.
The other advantage of ultrasound is that you can have a preliminary idea of the diffusion of a tumour. Ultrasound as a staging procedure gives a better idea of the skin and subcutaneous fat, especially when you have a tumour that is superficial. It’s very important for the surgeon to know if a tumour has invaded the superficial area. Between the skin and the gland there is the subcutaneous fat that includes some important ligaments. The Cooper ligaments are well known, but you also have a very thick ligament that runs parallel to the skin -- the superficial fascia -- and this is a barrier against the progression of both inflammation and tumours. For example, you may have a 5mm diameter tumour, which means a very low grade tumour, but it invades the fascia going towards the skin; in this case a tumour of 5cm is likely. So, because there is already an invasion of the superficial lymphatics, this is clearly seen with ultrasound.
The other possibility, to understand a little more in comparison with mammography, is to see if there is an extension in the ducts or if we have multifocal cancer. Really, MRI has been demonstrated to give better results and now is the gold standard for preoperative staging, but ultrasound can give an initial idea. ‘The other advantage is the possibility to evaluate the axilla, in the same examination, because ultrasound works very well in the axilla with lymph nodes. Today, not all centres, but a high percentage of them use it as the preliminary examination. You cannot really say that there are no pathological lymph nodes. But, if you do see them you can spare the sentinel node procedures with radiotracers, because you already know there is a node invaded by the tumour and, to be more certain, you can pick up some cells with cytology, for example, and say to the surgeon, “Okay, you already know that there’s an invaded node”, and you go directly for surgical axillary dissection. You don’t have to perform a sentinel node procedure. So, you save money and the operating theatre scheduling is better. Ultrasound is not the best examination for staging, but it’s better and better compared with mammography.
‘In the last three or four years we have seen huge technological advancements. First, medium-end technology, not only the high-end, has increased its quality. So you can have a basic ultrasound breast examination without spending too much money. That’s important, especially for some screening centres; they usually decide to spend a lot on mammography, but not so much on ultrasound. Usually, many European centres have very good mammographic units and very poor ultrasound technology. Now, things are changing, because they can buy medium-end technology and really they can perform a good basic examination. If you want a little more, you must go to more advanced technology.
‘There are three major points. You must have very good transducers, because transducer quality is crucial, and today you need a matrix transducer. For the breast, the frequency must go at least from 9 to 16 MHz. You must have a Doppler frequency inside to evaluate vascularity, and it must go up to 8 or 9 MHz, and even more.
‘Another point is the width of the scanning field. How large must be the transducer? If it is too small, you don’t have a good overview of the breast, so you need 4.5-5 cm footprint. With the new technology there is also the trapezoid image – electronically you can make the image wider, so you can explore the breast better in depth.
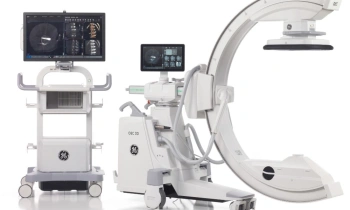
‘I work with GE’s LOGIQ 9, but I also have the new LOGIQ E9. It’s far more sophisticated than the LOGIQ 9. The major differences impacting the image quality are the innovative system Agile Acoustic Architecture and the quality of the transducers. First, the more powerful and sophisticated the computing capability of the platform, and the capabilities to change different parameters, the more information you can obtain. For example, with high-end technology you can move around very quickly through the breast using very sophisticated control. So you can use compound imaging that makes the margins of the lesions and the anatomical structure clearer, and you can suppress noise inside the image. So, the image is clearer and sharper, and you still can move very quickly because having a high computing capability, you can preserve a high frame rate per second and your eye is not disturbed. With lower technologies, you can move around very quickly, but at that point you have to take off all the controls that make the image clearer.
‘Next, the more sophisticated the technology the greater the possibility to evaluate the vascularity of a lesion, because the sensitivity to vascularity increases. I must say that perfusion imaging, using contrast agents, becomes better with high-end technology; but, from some companies, it’s not so bad in the medium technology.
‘In the LOGIQ E9, GE has done a very good job in image processing, because it has logged special algorithms that dynamically optimise the different imaging parameters to the selected acoustic profile to build the final image So, the image you obtain from the beginning is very good and need only minor adjustments when scanning. The final goal, which I think in the next focus is the possibility to consider the real time beam changes (as speed of transmission, attenuation) moving through different kinds of tissue. In ultrasound there’s an international standard to use a velocity of 1,530 metres per second. That’s not the sound velocity in all the tissues, but a sort of average velocity. For example, in the breast we can have gland in younger patients and a lot of fat in older patients. It’s not always true, but it’s the average rule. However, when the ultrasound waves are moving in the fat, the velocity is lower compared with the other velocity. So, the next step, for many manufacturers of high-end technologies, will be to consider the speed of sound changes in the examined anatomy to be able to perform a real time automatic compensation of the imaging parameters in transmission. At this point, you’ll reduce a lot of the noise as well as artifacts and have the best image at any time. The LOGIQ E9 is going in this direction.
‘Today, anti-tumour drugs have improved hugely, particularly the new anti-neoangiogenetic drugs to try to repair new tumoral vessels. In this case, ultrasound is very important, especially the use of contrast agents, because you can very quickly monitor whether those therapies are efficient or not. These new vessels have holes that load different enzymes to leave the vessels and to prepare and reduce the capability of the resistance of the surrounding tissues to the tumour. The gadolinium that is used in MRI can leave these holes, in the sense that it measures not only the perfusion inside the tumour, but also outside the tumour. On the contrary with ultrasound the bubbles do not go through these holes; they remain inside the vessels of the tumour, so I think the t is better measured with ultrasound.
We will see in the future what happens, but I must say that today the results obtained with ultrasound are quite incredible because after a few days you can understand if the drug is working, or not. The problem is that these drugs are very expensive, so you need something that allows you to understand it very quickly.
You can switch the therapy management if it doesn’t work. That is very important. I think, in the coming year, one of the major points will be which breast imaging you will use to monitor the efficacy of the therapies. So, to measure the volume of a nodule, requiring real time 3-D, as well as to measure the perfusion of the tumour before and after therapy, technology is very important. I think that, in the future, radiology will be more directed to monitoring the efficacy of the new therapies than only to the diagnosis.
07.03.2009
- breast cancer (629)
- elastography (89)
- mammography (259)
- MRI (836)
- ultrasound (769)
- women's health (339)