
© Africa Studio – stock.adobe.com
News • ABO antigen analysis
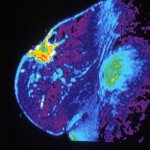
Blood type A identified as breast cancer risk factor
A comprehensive study, led by first authors Rahaf Alchazal from Yarmouk University and Khaled J. Zaitoun from Johns Hopkins University School of Medicine and Jordan University of Science and Technology, examined the potential link between blood type and breast cancer.
The research team conducted a systematic review and meta-analysis of 29 previously published studies, involving more than 13,000 breast cancer patients and over 717,000 controls. Researchers searched for studies on breast cancer patients and ABO blood groups across four major databases: PubMed, Scopus, Web of Science, and Google. Their insights were published in Oncotarget.
Breast cancer is the most common cancer among women worldwide. Identifying risk factors is vital for early detection and prevention. While many studies have explored lifestyle and genetic causes, this analysis focused on the ABO blood group system. By pooling global data, the researchers found that blood type A was the most common among breast cancer patients and was significantly associated with an 18% increased risk compared to type O.
Recommended article
Article • Research, diagnostics, treatments
Focus on breast cancer
Breast cancer (breast carcinoma; often abbreviated as BRCA) is the most common cancer in women in many countries and the cancer with the highest mortality rate. The diagnostic and therapeutic options for breast cancer are correspondingly diverse. Keep reading for latest developments in early detection, staging, treatment and research.
The study did not find a significant association between breast cancer and blood types B, AB, or Rh factor. Although the results do not prove causation, they point to a biological pattern worth further investigation. Blood group antigens are proteins found on the surface of cells, including breast tissue. These molecules may influence how cancer develops and spreads by interacting with the immune system or affecting cell behavior.
This meta-analysis is the most extensive review to date on this topic, based on studies conducted across Asia, Europe, Africa, and the Americas. While previous research found unclear conclusions, this large-scale evaluation provides stronger evidence for a possible connection between blood type A and breast cancer risk. Researchers note that regional differences, genetic diversity, and study quality may affect individual results. Nevertheless, the overall trend supports considering blood type A as a potential risk marker. This insight could help shape screening guidelines, encouraging earlier or more frequent checkups for women with this blood type.
Further research is needed to understand why blood type A may play a role in cancer development. Future studies may explore genetic mechanisms, immune responses, and other biological pathways. These efforts could lead the way for more personalized cancer prevention and care strategies.
Source: Oncotarget
16.05.2025





