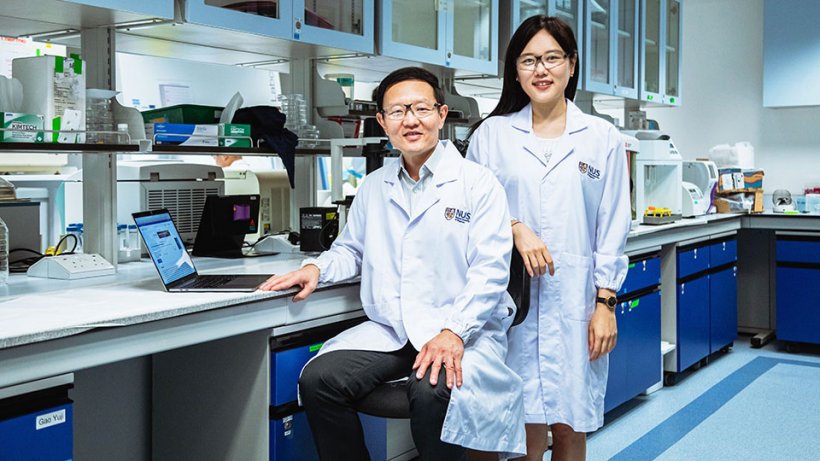
Image source: NUS
News • Tumour Matrisome Index (TMI)
Big data breakthrough in cancer diagnosis
A team of researchers from the National University of Singapore (NUS) has discovered a new personalised tool to detect cancer, predict patient survivability and how well a cancer patient would respond to immunotherapy.
This tool is a specially-designed cancer 'scorecard' to be used with the standard blood test for cancer (also known as liquid biopsy). This 'scorecard', which the team termed as the Tumour Matrisome Index (TMI), is a panel of 29 selected genes produced in the extracellular matrix (ECM) of the human body. ECM is the space around cells and provides structural and biochemical support to surrounding cells, behaving like a scaffolding. In a series of studies, the NUS team found that these 29 genes had appeared repeatedly as a consistent factor in patients diagnosed with non-small-cell lung cancer (NSCLC) which accounts for approximately 85 per cent of all lung cancers.
The team’s findings were published in two scientific journals — in the Proceedings of the National Academy of Sciences and in the Nature Partner Journal’s Precision Oncology.
This is a big step forward in personalising cancer treatment and ensuring better patient outcomes
Lim Su Bin
The research was led by Professor Lim Chwee Teck from NUS Biomedical Engineering and recent PhD graduate Dr Lim Su Bin. Prof Lim explained, “TMI can be used together with liquid biopsy, which is less invasive and less painful for the patient compared to conventional tumour biopsies. As it only requires a blood test instead of day surgery, it can be done more frequently over the course of treatment, providing doctors with real-time information on how the patient is responding to treatment. Tissue biopsy is often done at the start and end of treatment, while liquid biopsies can be done frequently, allowing doctors to track more efficiently how well treatment is progressing. This is a big step forward in personalising cancer treatment and ensuring better patient outcomes.”
To develop and validate the TMI “scorecard”, Dr Lim used big data and predictive analysis of over 30,000 patient-derived biopsies. “Parallel analyses in over 30,000 patient-derived biopsies revealed that the TMI scores are closely associated with mutational load, tumour histopathology, and predictive of patient outcomes,” she said.
Using public datasets of healthy individuals and cancer patients, the team noticed that cancer patients had a higher set of TMI scores. Testing a person’s TMI signature can determine if someone has cancer or not. They also examined the 29-gene TMI in 11 major cancer types - lung, pancreas, prostate, kidney, stomach, colon, ovary, breast, liver, bladder and melanoma. The team found that the TMI scores distinguish cancers from normal tissues, and that each cancer type has a specific TMI signature.
So far, the TMI signature can diagnose with certainty someone with lung cancer, but further validation is required for the other 10 cancer types.
Recommended article
News • Personalized diagnostics
AI checks effectiveness of immunotherapy
Scientists from the Case Western Reserve University digital imaging lab use Artificial Intelligence (AI) to predict which lung-cancer patients will benefit from expensive immunotherapy. This is done by teaching a computer to find previously unseen changes in patterns in CT scans taken when the lung cancer is first diagnosed compared to scans taken after the first 2-3 cycles of immunotherapy…
Predicting treatment effectiveness, survival and recurrence rate
The team also showed that TMI scores could be used to predict how successful a patient might react to cancer treatments, such as immunotherapy. Immunotherapy is the process where the body’s own cells are used to attack cancer cells as a form of cancer treatment. It is preferred over chemotherapy, which is more commonly used, as it is much less invasive and has shown to have better efficacy.
Cancer tumours can either spread to different parts of the body (metastasize) or return (recur) if unsuccessfully treated. Determining if a tumour is likely to metastasize or recur was previously a challenge as it is often done through macroscopic imaging techniques which could often be nonspecific. A patient’s TMI scores could give a better gauge on his or her survivability, the team found. In their work with NSCLC the team found that high TMI scores were consistently associated with early recurrence of cancer and metastatic spread, leading to an increased risk of death.
For cancers such as colon, liver, renal, and breast cancers, the higher the TMI scores, the higher the risk of cancer recurrence or metastasis, and hence, the lower the patient’s chances of survival. However, for gastric and ovarian cancers, the opposite holds true: the higher the TMI scores, the lower the risk of cancer recurrence or metastasis and the better the chances of survival. “There might be other factors in the gastro-intestinal microbiome, such as the presence of intestinal microflora, which affects the patient. This requires more study,” said Prof Lim.
Moving forward, Prof Lim and his team plan to collaborate with their clinical collaborators to conduct further clinical tests to validate the use of TMI on other cancer types. This will determine how accurate and specific TMI will be in the diagnosis and prognosis of patients via liquid biopsy or blood test. This has great potential in becoming a standard test not only in detecting cancer, but also predicting patient survivability.
Source: National University of Singapore (NUS)
15.01.2020





