Article • GCCA/GBCA safety
Gadolinium @ ECR 2018 – diverse and “disunited”?
Gadolinium-containing/gadolinium-based contrast agents (GCCAs/ GBCAs) and their usage was a major topic at ECR 2018. Fuelled by the current debate a number of presentations focused on possible impact, risks and necessities. Some were highly specific, others took a broader view. The only consensus, however, seems to be the need for more research and the focus on safety.
Report: Lena Petzold
How safe are gadolinium agents?

This question came up regularly at ECR 2018 but no clear-cut answer was found. Joseph Castillo, manager of medical imaging services in several hospitals on Malta, who filled in for Andrea Cradock, a MRI clinical specialist radiographer in Ireland, assessed the question based on her collection of historic and current observations:
Gadolinium has been applied for diagnosis and treatment guidance in almost 300 million patients worldwide*. After the first cases of nephrogenic systemic fibrosis (NSF) were reported in 2006, doubts rose, though only 170 cases were reported globally. In 2010, the first European Medicines Agency (EMA) report on the use of GCCAs was published, including risk assessments. In summary, the guidelines required macrocyclic agents to be used with patients found to have a high risk of NSF. In 2013, the first report of gadolinium deposits evident in the brain was published by Kanda et al(Article in german) who in 2015 also found that it was associated with past linear but not past macrocyclic chelate administration. Consequently, in March 2017, EMA’s Pharmacovigilance and Risk Assessment Committee (PRAC) declared macrocyclic agents as safe but recommended to restrict the use of several linear agents and to suspend the authorisation of three linear agents. In November 2017, the European Commission confirmed these guidelines and rendered them applicable to all EU member states.
So where do we go from here?
We need to avoid gadolinium-based contrast agents as far as possible during our scans, thus we need to revisit our protocols and use better protocols that now exist on the market.
Joseph Castillo
After having established the historic baseline, Joseph Castillo advised on behalf of Andrea Cradock: “For sure, we need to stick to what is evidence-based. We need to avoid gadolinium-based contrast agents as far as possible during our scans, thus we need to revisit our protocols and use better protocols that now exist on the market.” He also suggested the application of other appropriate techniques such as high-tesla imaging or susceptibility weighted angiographies (SWAN) for the detection of multiple sclerosis. Castillo further recommended following the guidelines, applying them as necessary to the clinical scenarios and keeping abreast of as well as conducting more research, particularly in view of the fact that important findings have surfaced: “Recently, traces of gadolinium have been found in the water supply.” Thus he called for healthcare professionals to consult with environmental experts to determine the clinical consequences of this development, “because you can have T1 hypersensitivities in your brain without ever having undergone an MRI scan”.
Should we avoid linear agents because of intracranial retention?

Dr Howard A Rowley, professor of radiology, neurology, and neurosurgery at the University of Wisconsin, USA, presented a less restrictive approach and concluded: GCCAs are indeed quite safe and have great benefits.
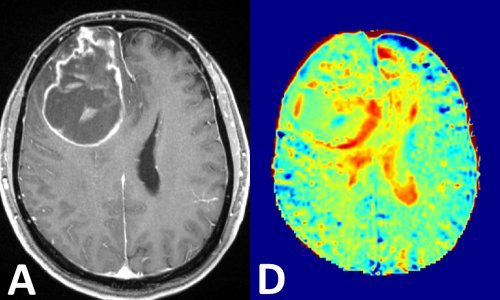
Gadolinium deposition in tissue has been described in animal models since at least 1984. Yet the ‘rediscovery’ of this fact and the ensuing debate managed to have a great impact especially in the EU, outlined Rowley. He disagreed with the EU Commission’s suspension decision that he believed was based on the assumption that there are other agents and solutions that can do as well as linear GCCAs. In Rowley’s opinion, there is no viable alternative yet, especially in terms of relaxivity. He supported his point citing the results of multiple studies confirming that for example MultiHance performed better than any of the other agents for brain tumor work, contrast-enhanced MRA, or with Breast MRI. In the USA multiple agents are still in use and Rowley declared them indispensable for different applications such as vascular imaging or parenchymal imaging.
Linear agents are indispensable – and they are not all the same.
Dr Howard A Rowley
GCCAs are quite safe agents, he said, they have excellent safety profiles and they all share a similar and typically low acute adverse event rate, below one percent. He did not overlook the occurrence of NSF but rather pointed out that NSF is a “success story” from a regulatory standpoint, because “through regulatory action and through science we were able to essentially eliminate it.” He also noted that the agent with highest relaxivity (MultiHance) also has no reported cases of NSF, conferring both safety and efficacy advantages over other agents – yet as a linear agent it is no longer available for general use in the EU.
What about gadolinium retention?
“We’re puzzled at what happened here with the PRAC and EMA,” Rowley conceded. Gadolinium retention is an asymptomatic phenomenon – not a disease – that has been seen with all agents since the 1980s but triggered a response that though well-intended and precautionary basically promoted the death of several linear agents. He alleges that the risk-benefit analysis has not been properly considered. The benefits have not been assessed appropriately while “as far as I can tell, the real world clinical risk of this is zero”. The unintended consequences of the debate and the suspension were great, he continued, not only did they create bad press for all of the agents, but they also led to a gadolinium phobia and patients refusing necessary examinations. “We’re seeing lawsuits and blame and pointing of fingers,” he said but also stressed that “hopefully it will be one of those good controversies that will bring us together to try to sort this out.” Rowley reminded the audience that metal deposition in the brain is normal, for example iron deposition is seen on T2* MRI sequences in people of all ages.
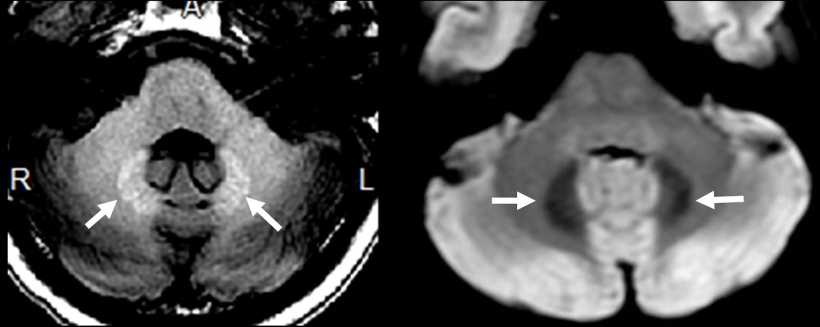
He also presented several recent studies that found neither neurologic outcomes nor cognitive decline linked to gadolinium deposition nor a connection between gadolinium and Parkinson’s (Welk JAMA 2016). However, he also concluded that much more research on absorption and distribution processes as well as on potential toxicity and trafficking is needed to fill the knowledge gaps and recommended to use gadolinium wisely and individually. So is gadolinium deposition a threat or a phantom debate? Read more about it here.

Are there issues that the debates are not covering?
Paul M Parizel, chairman of Antwerp University Hospital’s department of radiology in Belgium, also commented on the reappearance of the issue of gadolinium deposition. Parizel, who on short notice replaced Robert J McDonald, MD, PhD, a senior associate consultant at the division of neuroradiology at Mayo Clinic in the USA, asked whether we are “reinventing the wheel?” on behalf of McDonald, stating that already back in 1984 healthcare professionals knew that residual gadolinium was found in the kidney, liver spleen and other tissue and that since then intracranial gadolinium deposition has been detected in every GCCA-exposed patient tested to date. The renewed rather “explosive” interest however disregards several aspects according to McDonald.
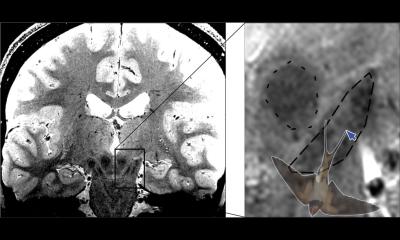
Most importantly, he questioned the depiction of macrocyclic agents as the ‘completely safe’ option. Recent animal studies performed at the Mayo Clinic and in Italy show that gadolinium tissue concentration is not entirely class-dependent and that there are also interclass differences in macrocyclic agents. All GCCAs are to some extent retained in the body. According to McDonald, the imbalance in favour of macrocyclic agents results partly from too many studies focusing on T1 signal data rather than on mass spectroscopy results. “There is evidence of macrocyclic deposition despite negative T1 results in preclinical animal models,” Parizel stated on behalf of McDonald, pointing out that mass spectroscopy seems to be more sensitive to detect microscopic amounts of gadolinium deposition and that the T1 shortening only starts to be seen with higher amounts. McDonald therefore urges researchers to focus on quantitative tissue analysis rather than on the T1 signal; especially since lack of standardization of T1-weighted sequences between scanners and institutions makes comparisons difficult and results unreliable.
Refocusing on science
As we try to determine if GDD is genuinely causally related to long term gadolinium deposits, we need to be diligent as scientists.
Robert J McDonald, MD, PhD
McDonald also emphasized a larger scientific concern in the debate: “We must avoid temptation to cherry-pick data.” Thus, studies need to be fine-tuned since for example one of the highly debated topics, gadolinium deposition disease (GDD), a term coined by authors from UNC in Chapel Hill North Carolina, was based on an uncontrolled survey and self-reported data of a very small subset of patients who had already self-attributed their symptoms from prior GCCA exposure. Gadolinium deposition remains a nascent field of study and should be analysed intensively, but McDonald underlined that so far extensive research could not find any histologic changes noted in brain, liver or spleen. Other reassuring assessments include the Mayo Clinic study of Aging (MCSA, 2004 till current), a large population-based study on dementia, which “accidentally” studied the effects of gadolinium deposition for more than ten years finding no effect of exposure or dose-response relationship on cognitive function in this population. To date, these findings suggest that gadolinium deposition does not appear to have significant adverse clinical effects. However, according to McDonald, more research is needed in the clinical effects of gadolinium deposition as each study adds incrementally to the body of knowledge on this subject and current studies cannot completely exclude the possibility of extremely rare or subtle clinical effects like those reported in GDD. “As we try to determine if GDD is genuinely causally related to long term gadolinium deposits, we need to be diligent as scientists,” McDonald pointed out and emphasized that, “both linear and macrocyclic agents should be scrutinized as both have been causally implicated in this clinical entity.”
Want to know more? Read why science is so important for the discussion.
* Author’s note: numbers varied slightly across lectures
Profiles:
Joseph Castillo manages the medical imaging services across Malta and Gozo on Malta, including Mater Dei Hospital and Gozo General Hospital.
Andrea Cradock is a MRI clinical specialist radiographer and lecturer at the University College Dublin, Ireland.
Dr Howard A Rowley is professor of radiology, neurology and neurosurgery as well as Chief of Neurological MRI and the Joseph F. Sackett Professor of Radiology at the University of Wisconsin School of Medicine and Public Health, USA.
Paul M Parizel is chairman of Antwerp University Hospital’s department of radiology in Belgium and full professor of radiology at the University of Antwerp’s Faculty of Medicine and Health Sciences.
Robert J McDonald, MD, PhD is a senior associate consultant and assistant professor of radiology in the department of radiology at Mayo Clinic in Rochester, Minnesota, USA.
13.04.2018